- Joined
- Dec 22, 2018
- Messages
- 583
- Reaction score
- 1,613
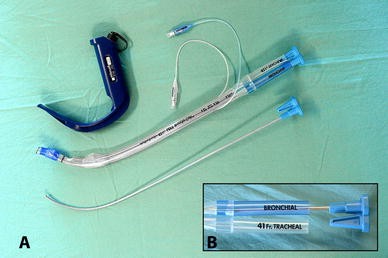
What do you all consider the best approach in patients who need a DLT, and have a grade 3/4 view upon DL? Assuming bronchial blocker isn’t an option (surgeon’s strong preference, need to flip back and forth between 2 lungs during OLTx, etc). I usually end up going single lumen —> tube exchanger (the long skinny one with a purple floppy end, vs one of the Cook airway exchange catheters). But, this isn’t always as easy as I’d hope. I’ve not had good luck at all with glidescope or CMAC - Usually get a good video view but not enough working space for the tube.
Any tricks up your sleeve? Always open to learning new things. Have heard McGrath is better for DLTs given the low profile, but don’t have them at my institution.
Any tricks up your sleeve? Always open to learning new things. Have heard McGrath is better for DLTs given the low profile, but don’t have them at my institution.