- Joined
- Oct 17, 2023
- Messages
- 219
- Reaction score
- 268
- Points
- 116
I respectfully disagree.I do not think labor epidurals are in anyway similar to what we do, and I did a lot of thoracic catheters for CT surgery and trauma during my fellowship. We did acute pain, and yes I went in at 0300 to place bedside catheters in polytrauma pts. It has nothing to do with our field IMO.
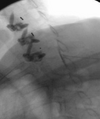
I did about 15 epidurals a night. I learned how to calm the patient, how positioning is important, how to manage the room, how to check for complications, how to set up my tray, how to anticipate my next move, how to consider different injectates and most importantly how to appreciate using fluoro and taking my time which are two luxuries one doesn’t have on the L&D floor.