I get criticized for overly loquacious posts. So I will try to be succinct by way of analogy. The
tilt-a-couch (how about just setting up the patient well, measuring the rot error with IGRT, and if <1° pitch/yaw/roll, don't need 6DoF couch?), the leaves, the margins, the isocenter number(s)... they are all versions of
Walter White's fly. When the meth is ~99% pure, a tenth a percent either way is angels dancing on the head of a pin. Wanna chase the fly? Chase it! Wanna get the meth out? Get it out!
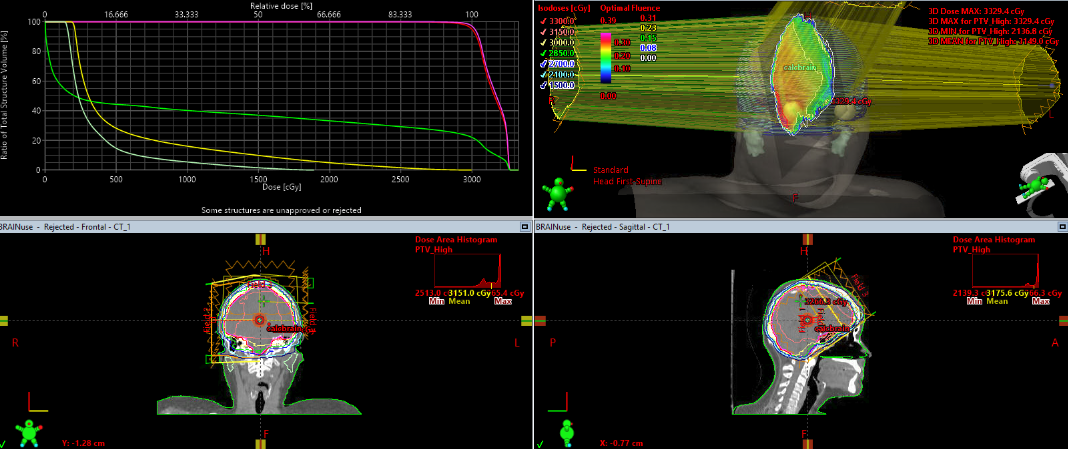
I disagree. 1 degree of rotational error magnifies. From trigonometry, if your isocenter is 7 cm from the target, 1 degree of rotational error gives 1.2 mm of translation. So what is your PTV? 0-1 mm of PTV might be sufficient if you're precise enough in patient position. But if your isocenter is further away or rotation is more than 1 degree... Now you've missed part or all of the target.
I don't believe in going bigger than 1 mm PTV because then I'm just going back to GK or multi-isocentric linac treatments. IMO, what is the point of doing SRS if your margin is 2-3 mm?
If you only do 3D couch corrections with an isocenter far from some of your targets, the rotation errors can absolutely still be uncorrected and you miss part or all of your target again. If you're not using a 6-DOF couch, I think you should absolutely set a limit to how far a target can be from your isocenter. Hyperarc and many related SRS techniques will often put your isocenter well away from at least some of your targets, so you need to be aware of that.
agree with most of what you are saying- especially point 5 re fusion accuracy (i also find contrast helps with these fusions and sometimes have seen different enhancement patterns on ct and MRI including several instances where the ct enhancement was larger than that seen on mri). For insurance and logistic reasons, getting timely spatially corrected volumetric mri can be difficult, and when this is an issue, it does sway me to add margin, and when I add margin, I fractionate.
I don't treat unless I have an MRI within 14 days of treatment, preferably within 7. There is data showing worse outcomes when the MRI is older than 13 days. I have seen lesions grow several mm in two weeks, and so if your MRI is older than that you are straight up guessing about growth at that point. That's a hard no for me.
I have been using UAB approach for 4-5 years now.
When I talked to the UAB folks they have always used microMLC. My impression is that they don't understand why anyone would do these treatments without microMLCs.
Do differ on extent to which micro mlcs have impact on plan for small lesions. Scarbtj probably could comment more, but with single iso vmat 1) many of lesions seeing dose delivered by larger peripheral 5mm mlcs away from the 2.5 central micromlc? 2) collimator rotations really lessen effect of mlc size. I dont have hyperarc, but would love to get it and play around with it.
I ran a lot of plans with microMLC vs. regular MLC to justify the cost of a microMLC equipped linac. For tiny lesions there is a huge difference in metrics like conformity and gradient index. But for all lesions, you add on the order of 0.6 - 1.0 cc of V12 for every lesion treated with regular MLCs compared to microMLC, and this holds up even for large lesions. So if you treat a 15 small brain met case, now you've added ~10 cc of V12 to the entire brain. This might actually disqualify a patient from CE.7 trial which limits whole brain V12 to 30 cc. Now does this whole brain V12 actually matter when it's scattered throughout the brain? I don't know. But I don't really want to find out either.
As for your point about larger peripheral MLCs, it's the center 16 cm that gets the HDMLCs. So usually the lesions will be in there. But you have to decide whether you'll accept some being treated by the standard MLCs (UAB does, and it's a minority of lesions obviously). As for point 2, not sure what you're referring to. Maybe I'm unaware of something.

 www.ncbi.nlm.nih.gov
www.ncbi.nlm.nih.gov


 If you convert them, get ready to train them in how to draw the hippocampus, the dosimetrists in how to generate the plans, and how to prescribe memantine.
If you convert them, get ready to train them in how to draw the hippocampus, the dosimetrists in how to generate the plans, and how to prescribe memantine.