This is a brief reddit thread from about 10 months ago. Based on reading the comments, it seems like the comments are from med students and PGY1 interns mostly. The negative nephrology vibes are already entrenched in this younger medical professional population. There is no hope for the ASN. #STARTreks and #NephMadness lol. please.
Let's dissect a few of these responses.
When it comes to newly minted clinical educators in an academic set up for a nephrology, this is a spot on statement. I will also add that the nephrologist is more at the mercy of the Cardiothoracic Intensivist (the extension of the surgeon) than the Cardiologist.
On the flip side, this is a M-4 who probably only sees the fellowship and large academic center faculty physicians. Therefore, I can see where this bias stems form.
Yep sounds like a med student who doesn't have any loans to pay back and whose parents have an educational savings fund. $175K in a large metro are will NOT cut it. One can argue that the residency /fellow salary like 60-80K might be better because they have education, food, and housing stipends.
The peds neph job sounds right on the money. Academics do pay less. It's not just nephrology. In general academics pays less than PP. Because in PP, you are the hunter and if you hunt more, you eat more. If the private groups are poaching consults from the faculty group, then the hospital cannot justify the (already low) salary of the academic group and will force cuts or force more business (hence the fellow comes in for all BS consults). As for those PP jobs... well yes... but not everyone can get those. See this entire thread.
You're not wrong about the first line. I often thought that the renal fellow works almost as hard as the cardiology fellow (CCU in house night call vs out of house night call but need to come in for HD is a toss... depends on volume) but gets far less kudos and reward down the line.
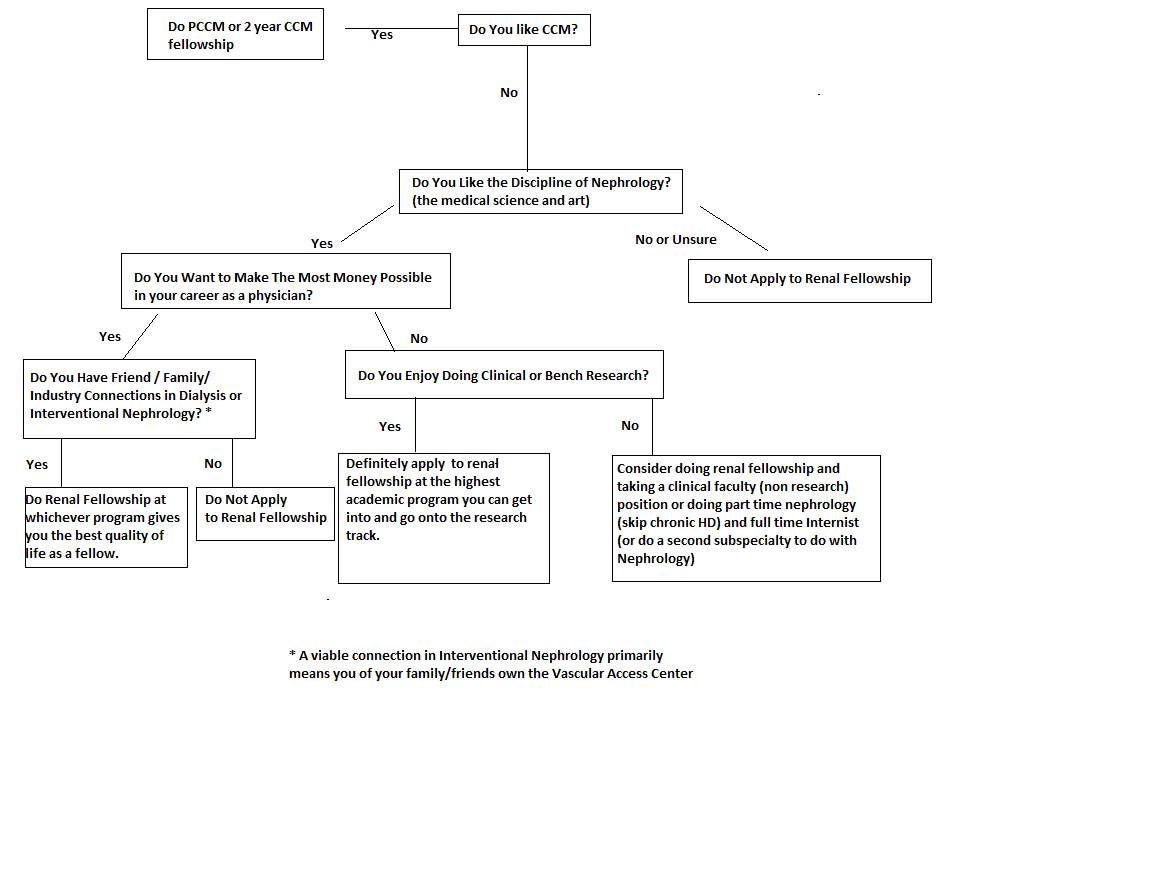
As for the ownership of the dialysis center, I will say Renal Prometheus will have more to say about this (see prior posts also)
This is probably the most accurate statement describing a "thriving" private practice nephrologist.
This is also a fair statement. But this is a med student who did an academic nephrology rotation. Therefore you bet they will have seen a lot of GN, transplant, and systemic "cool House MD" kind of cases. This is NOT what happens in private practice. One could be an academician, maybe do renal transplant subfellowship, etc... and then be a Dr House. House MD did "dual residencies" in Nephrology and Infectious Disease. That shouldn't be a very hard combination to achieve in real life.
Yep pretty much. Though to be fair, the inpatient HD patients are the real trainwrecks and IM residents often get a kind of selection bias that all HD patients are trainwrecks. There are "thriving" HD patients who actually avoid hospitalizations and seem "normal." But only the nephrologists see those patients outside.
Money cannot buy happiness. But being broke can lead to depression. Life's unfair.
Yes, this is the thesis of my posts within this thread.