What's the gauge and max flow rate on your CVL? A lot of times a large bore peripheral is larger gauge with a much higher flow rate than some of the central catheters (but, I'm sure you know that). 22g is not adequate for resuscitation. A much larger bore might be. The fact the the line is "central" means nothing alone, from the standpoint of max flow rate. It's all about the catheter size (but, I'm sure you know that). It drives me
insane when someone puts in some teeny weeny little angel-hair-noodle
central line and they think it's real aggressive because it's "closer to the heart," or because it has multiple lumens, when they don't even know the gauge. Nurses will sometimes reflexively go to a smaller bore in a crisis because they feel they have a higher success rate on placement, but you may be stuck with something so small it has pathetic flow.
I'm going to invent a 5 lumen central line, and it will sell. Why? For the same reason the amazing
7-blade razor sells like hot cakes, at 20 times the price. Because it has......
More.
Yeah....more, of anything. Next year, I'll do the shocking, and unexpected. In a secret reveal, with all media present, I'll debut the
6-lumen catheter to dropped jaws. (Secretly, I will have a 7 lumen in the pipeline for the year after that).
"7 lumens = 7 times
better"
(But, "shhh...!") Not any faster for resuscitation.
Absurd? Yes, but demonstrates the absurdity of being wowed by gadgets and the fancy (devices with cool names, bells and whistle, but aren't proven to work any better), over things that are really important, like a couple boring, not so flashy large-bore peripherals that can be placed by anyone, and
don't need to be placed by anyone with fancy, super-duper cool skills and lots of fancy letters, titles, and new "protocols."
(8 lumens? Don't you dare even think about it. It can't be done!)
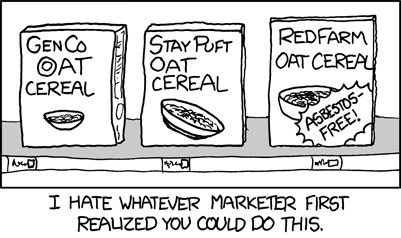
Another example of how we are absolute fools for "the fancy," without demanding any proof of "better":
Da Vinci robot:
http://www.medscape.com/viewarticle/802971