PPS exemption is the biggest pile of horsesh__ in our field, and it's not even close. Until this is addressed, the #financialtoxicity #choosewisely crowd has no moral ground to stand upon.I'm trying to stay positive, but reading this thread and learning more about APM has got me down....
Say my radiation center is in an APM zip code and also next to a PPS-exempt center.
If a patient gets treated for a bone met by me and within 90 days has another bone met, if I
A) don't treat, patient suffers
B) treat them, I will not get paid for additional services
C) send patient to the PPS-exempt center for treatment that will still get paid (and likely steal my patient), and it ultimately doesn't save CMS any money. After CMS does not save any money, I would hope that it scraps this silly experiment, but the more likely scenario is that it finds more ****ty ways to squeeze little rad onc.
Am I understanding this correctly? If so, this is a no-win situation...feels sickening.
Rad oncs have talked a lot about anti-trust with residency numbers. What about this blatantly anti-competitive PPS-exempt non-sense? Such incredibly unfair advantages to being exempt. Going to be a lot harder to spend money for new technology if our reimbursements are getting slashed. Meanwhile, PPS-exempt center is building proton center #2. This can't be legal?
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
RO APM Dies!
- Thread starter domestique
- Start date
- Joined
- Apr 3, 2019
- Messages
- 4,263
- Reaction score
- 9,929
While people were arguing about whether forward planning was true IMRT, or 45 vs 28 fractions for prostate, or RT avoidance in old women with breast cancer...I'm trying to stay positive, but reading this thread and learning more about APM has got me down....
Say my radiation center is in an APM zip code and also next to a PPS-exempt center.
If a patient gets treated for a bone met by me and within 90 days has another bone met, if I
A) don't treat, patient suffers
B) treat them, I will not get paid for additional services
C) send patient to the PPS-exempt center for treatment that will still get paid (and likely steal my patient), and it ultimately doesn't save CMS any money. After CMS does not save any money, I would hope that it scraps this silly experiment, but the more likely scenario is that it finds more ****ty ways to squeeze little rad onc.
Am I understanding this correctly? If so, this is a no-win situation...feels sickening.
Rad oncs have talked a lot about anti-trust with residency numbers. What about this blatantly anti-competitive PPS-exempt non-sense? Such incredibly unfair advantages to being exempt. Going to be a lot harder to spend money for new technology if our reimbursements are getting slashed. Meanwhile, PPS-exempt center is building proton center #2. This can't be legal?
the asteroid hit.
- Joined
- Oct 4, 2017
- Messages
- 5,015
- Reaction score
- 9,781
Astro board member Ben Smith criticizes imrt for breast as financially driven, yet pushes protons at a pps exempt center, charges 10 x cms rates, and once claimed that there would be a shortage of radoncs, laying groundwork for residency expansion. Quintessential IYI- these people are a real piece of workPPS exemption is the biggest pile of horsesh__ in our field, and it's not even close. Until this is addressed, the #financialtoxicity #choosewisely crowd has no moral ground to stand upon.
- Joined
- Sep 20, 2004
- Messages
- 11,734
- Reaction score
- 11,827
In third world countries you can bribe a police officer/dmv agent to get things done.I'm trying to stay positive, but reading this thread and learning more about APM has got me down....
Say my radiation center is in an APM zip code and also next to a PPS-exempt center.
If a patient gets treated for a bone met by me and within 90 days has another bone met, if I
A) don't treat, patient suffers
B) treat them, I will not get paid for additional services
C) send patient to the PPS-exempt center for treatment that will still get paid (and likely steal my patient), and it ultimately doesn't save CMS any money. After CMS does not save any money, I would hope that it scraps this silly experiment, but the more likely scenario is that it finds more ****ty ways to squeeze little rad onc.
Am I understanding this correctly? If so, this is a no-win situation...feels sickening.
Rad oncs have talked a lot about anti-trust with residency numbers. What about this blatantly anti-competitive PPS-exempt non-sense? Such incredibly unfair advantages to being exempt. Going to be a lot harder to spend money for new technology if our reimbursements are getting slashed. Meanwhile, PPS-exempt center is building proton center #2. This can't be legal?
In the US, you bribe the government. Big pharma has better lobbyists than rad onc and big rad onc/hospitals have better lobbyists than little rad onc/freestanding centers
D
deleted941485
In third world countries you can bribe a police officer/dmv agent to get things done.
In the US, you bribe the government. Big pharma has better lobbyists than rad onc and big rad onc/hospitals have better lobbyists than little rad onc/freestanding centers
More insightful than all the other nonsense I’ve heard about APM over the last year.
D
deleted941485
I think a lot of the problems that this field faces is the fact that there is such a strong divide between the Hospital and academic mega centers and small community and PP centers. As times changed, those interests widely diverged In a way that I don’t think exists in other specialties.
- Joined
- Apr 3, 2019
- Messages
- 4,263
- Reaction score
- 9,929
Hate to pick on ASTRO (again) but:I think a lot of the problems that this field faces is the fact that there is such a strong divide between the Hospital and academic mega centers and small community and PP centers. As times changed, those interests widely diverged In a way that I don’t think exists in other specialties.
1) ASTRO picked on private practice with Urorad brouhaha. I'm sure we could all tell a story or two about academic sites whining about losing prostate patients to PPs way back when.
2) ASTRO picked on private practice by the fake sanctimony of telling everyone "keep it down with the IMRTing" knowing full well that non-IMRT work on the academic side was getting reimbursed at rates far higher than IMRT in PP.
3) Once all academic/hosp centers became general supervision, when ASTRO says all of RT should be direct supervision they are in essence, again, only picking on PP.
One day, I hope, rad oncs will see that a call for increased control (Palliative Care Network?!?) or decreased reimbursement for one of us is a call for more control and less money for all of us.
- Joined
- Sep 20, 2004
- Messages
- 11,734
- Reaction score
- 11,827
4) opposed payment reform/bundled payments for several years while freestanding centers absorbed most of the cuts and many ASTRO member institutions were in a protons arms race with each other based on flimsy/no data to support itHate to pick on ASTRO (again) but:
1) ASTRO picked on private practice with Urorad brouhaha. I'm sure we could all tell a story or two about academic sites whining about losing prostate patients to PPs way back when.
2) ASTRO picked on private practice by the fake sanctimony of telling everyone "keep it down with the IMRTing" knowing full well that non-IMRT work on the academic side was getting reimbursed at rates far higher than IMRT in PP.
3) Once all academic/hosp centers became general supervision, when ASTRO says all of RT should be direct supervision they are in essence, again, only picking on PP.
One day, I hope, rad oncs will see that a call for increased control (Palliative Care Network?!?) or decreased reimbursement for one of us is a call for more control and less money for all of us.
- Joined
- Apr 28, 2005
- Messages
- 1,196
- Reaction score
- 3,433
From Astro published Sept 15th:
"Value-based payment has been the elusive holy grail of health care for the past decade. Many have laid the groundwork to establish payment models that seek to achieve the synchrony of improved patient care combined with cost savings achieved by identifying inefficiencies of one type or another. During this time, no professional society or medical specialty has pursued an alternative payment model (APM) more aggressively than the American Society for Radiation Oncology (ASTRO).1 As integral contributors to the care of patients with cancer, radiation oncologists provide high-value therapy with reliably favorable impact in a broad range of settings. Ensuring access to radiation therapy as part of the continuum of cancer care is particularly critical because of the significant growth in new systemic therapies, many of which do not represent high-value cancer care.2-5 Given the current structure of proposed federal payer APMs, however, there is concern that excessive reimbursement cuts threaten the capacity to sustain cancer patient access to radiation treatments proven to improve quality of life and overall survival."
"In the proposed rule, CMS recommended a 4% discount off of the Professional Component (PC) and a 5% discount off of the Technical Component (TC) payments. In the final rule, the CMS reduced the discount by a meager 0.25% to a 3.75% discount off the PC and 4.75% discount off the TC."
"Additionally, over the past 10 years, radiation oncology total allowable charges have represented a declining portion of the total Medicare Physician Fee Schedule (MPFS) allowable charges. The overall $47 million USD, or 3% decline, in allowable radiation oncology charges between 2010 and 2020 pales in comparison to the overall $15.7 billion USD, or 17% increase, in total MPFS allowable charges over the same period. This demonstrates that radiation oncology is not the driver of growing health care expenditures in the United States and should not be a target for rate reductions. Radiation oncology has proven itself to be a high value form of cancer treatment. That value should not be eroded through the application of severe cuts that will reduce access to care."
"Value-based payment has been the elusive holy grail of health care for the past decade. Many have laid the groundwork to establish payment models that seek to achieve the synchrony of improved patient care combined with cost savings achieved by identifying inefficiencies of one type or another. During this time, no professional society or medical specialty has pursued an alternative payment model (APM) more aggressively than the American Society for Radiation Oncology (ASTRO).1 As integral contributors to the care of patients with cancer, radiation oncologists provide high-value therapy with reliably favorable impact in a broad range of settings. Ensuring access to radiation therapy as part of the continuum of cancer care is particularly critical because of the significant growth in new systemic therapies, many of which do not represent high-value cancer care.2-5 Given the current structure of proposed federal payer APMs, however, there is concern that excessive reimbursement cuts threaten the capacity to sustain cancer patient access to radiation treatments proven to improve quality of life and overall survival."
"In the proposed rule, CMS recommended a 4% discount off of the Professional Component (PC) and a 5% discount off of the Technical Component (TC) payments. In the final rule, the CMS reduced the discount by a meager 0.25% to a 3.75% discount off the PC and 4.75% discount off the TC."
"Additionally, over the past 10 years, radiation oncology total allowable charges have represented a declining portion of the total Medicare Physician Fee Schedule (MPFS) allowable charges. The overall $47 million USD, or 3% decline, in allowable radiation oncology charges between 2010 and 2020 pales in comparison to the overall $15.7 billion USD, or 17% increase, in total MPFS allowable charges over the same period. This demonstrates that radiation oncology is not the driver of growing health care expenditures in the United States and should not be a target for rate reductions. Radiation oncology has proven itself to be a high value form of cancer treatment. That value should not be eroded through the application of severe cuts that will reduce access to care."
- Joined
- Apr 28, 2005
- Messages
- 1,196
- Reaction score
- 3,433
I'm not sure why Astro decided to pursue APM so aggressively (ie essentially volunteering for it and hoping for the best?). Seems like yet another big time error in judgement by our professional society.
I think the idea was that, if this was done in a non-destructive way through CMS, it would trickle down to private insurance and ease the burden of prior auths. Fractionation would become purely a scientific/logistical question; and you wouldn't have to go nine rounds on a P2P if an odd palliative case would be best treated with IMRT.I'm not sure why Astro decided to pursue APM so aggressively (ie essentially volunteering for it and hoping for the best?). Seems like yet another big time error in judgement by our professional society.
I think a non-destructive APM would probably really help a lot of PP, where having a huge cadre of billers may not be profitable.
- Joined
- Sep 20, 2004
- Messages
- 11,734
- Reaction score
- 11,827
We should have unhitched our reimbursement wagon from the per fraction model a long time ago. ASTRO resisted it while fraction shaming without thinking things through, while many in the freestanding community had been pushing for payment bundles since they were taking the worst cuts.I'm not sure why Astro decided to pursue APM so aggressively (ie essentially volunteering for it and hoping for the best?). Seems like yet another big time error in judgement by our professional society.
ASTRO absolutely should have embraced it awhile back and made it so all of their membership could be on the same foot. Hypofractionation is great for patients but should not penalize radiation oncologists and threaten the financial viability of a center for doing the right thing
The problem is ASTRO does not represent everyone in the specialty, esp those outside of large academic systems and now that CMS is essentially shoving it down everyone's throat without ASTROs blessings, they are trying to reinvent the narrative
- Joined
- Apr 28, 2005
- Messages
- 1,196
- Reaction score
- 3,433
"I think the idea was that, if this was done in a non-destructive way through CMS, it would trickle down to private insurance and ease the burden of prior auths. Fractionation would become purely a scientific/logistical question; and you wouldn't have to go nine rounds on a P2P if an odd palliative case would be best treated with IMRT.
I think a non-destructive APM would probably really help a lot of PP, where having a huge cadre of billers may not be profitable."
Sure. But it seems like there was a fundamental misunderstanding that the only purpose of APM is for the government to pay less for rad onc services.
I think overall bundling would make a lot of sense if done in a revenue neutral sort of way but then there would really be no point to this whole exercise from a payers perspective.
I think a non-destructive APM would probably really help a lot of PP, where having a huge cadre of billers may not be profitable."
Sure. But it seems like there was a fundamental misunderstanding that the only purpose of APM is for the government to pay less for rad onc services.
I think overall bundling would make a lot of sense if done in a revenue neutral sort of way but then there would really be no point to this whole exercise from a payers perspective.
- Joined
- Nov 2, 2019
- Messages
- 3,495
- Reaction score
- 14,489
Totally agree, keeping our reimbursements tied to fractions makes things so difficult. This paper just came out, which I haven't seen make as big of a splash as I would think (though perhaps I'm just in the wrong circles in the moment):We should have unhitched our reimbursement wagon from the per fraction model a long time ago. ASTRO resisted it while fraction shaming without thinking things through. They absolutely should have embraced it awhile back and made it so all of their membership could be on the same foot. Hypofractionation is great for patients but should not penalize radiation oncologists and threaten the financial viability of a center for doing the right thing
The problem is ASTRO does not represent everyone in the specialty, esp those outside of large academic systems
Increasing demand on human capital and resource utilization in radiotherapy: The past decade
Looking at the time period of 2012 through 2019, they found that "time-based human resources increased by almost 150%".
We've just really created the perfect storm of issues, where we churn out Radiation Oncologists, while still billing by the fraction, in an era where everyone is trying to cut (or eliminate) fractions, while the actual time each case takes is significantly more than it ever has been.
Meanwhile, ASTRO makes the assumption that if they give the government an inch, they won't take a mile. When in human history has that ever worked out?
- Joined
- Sep 13, 2021
- Messages
- 2,023
- Reaction score
- 2,263
'I'm from CMS and I'm here to help'
truth is, IMO, whether ASTRO or any one of us played ball or not, it was happening. ASTRO and their business committees (many of whom are in PP btw) decided it was better to try to be part of it than not.
truth is, IMO, whether ASTRO or any one of us played ball or not, it was happening. ASTRO and their business committees (many of whom are in PP btw) decided it was better to try to be part of it than not.
- Joined
- Sep 13, 2021
- Messages
- 2,023
- Reaction score
- 2,263
for example look at this paper
Hartsell - ROC, PP
Mohideen - well known chicago PP
Thaker - active, young PP health business guy
Vivek Kavadi - TOPA
Why does prostate pay so much more than lung, and more than H&N?This is a fascinating document... and frankly above my paygrade to understand completely. Being an employed doc; I quickly typed in the approximate professional fees per diagnosis from the national base rates. {This is not the overall payment, that has a way more complicated formula!}. It's going to be an interesting new economy. Three bone mets > cervical cancer ! Pivoting our clinical resources to increase throughput and efficiency for palliative cases may be quite worthwhile!
Dz Prof(hundreds) Bone Brain Lymph Breast Liver Lung Colorectal Pancreatic Uterine CNS UpperGI Bladder Anal HN Prostate Cervical
- Joined
- Apr 3, 2019
- Messages
- 4,263
- Reaction score
- 9,929
Because CMS has, since the dawn of routine IMRT, historically paid more for RT for the prostate cancer ICD code than for lung and H&N. Purely because fractions.Why does prostate pay so much more than lung, and more than H&N?
- Joined
- Sep 20, 2004
- Messages
- 11,734
- Reaction score
- 11,827
Why does prostate pay so much more than lung, and more than H&N?
ASTRO several years ago had look into splitting imrt planning codes into "simple" and "complex" as a way to screw urorads center. As absurd as it was on the face of it, it did seem to have some merit when you consider how much more work a gi or h&n plan can be compared to a standard IMRT N0 prostate, esp when those 44 fx pts were making bank for everyone owning a piece of said center.Because CMS has, since the dawn of routine IMRT, historically paid more for RT for the prostate cancer ICD code than for lung and H&N. Purely because fractions.
Then again, not a peep about protons for years now, since ASTRO clearly knows who is buttering its bread
- Joined
- Jan 26, 2017
- Messages
- 87
- Reaction score
- 218
Straight from the horses mouth:
- Joined
- Apr 21, 2011
- Messages
- 3,620
- Reaction score
- 9,243
Not a single MD on the author list. But there's always a BSN telling you what's going to happen.Straight from the horses mouth:
- Joined
- Apr 21, 2011
- Messages
- 3,620
- Reaction score
- 9,243
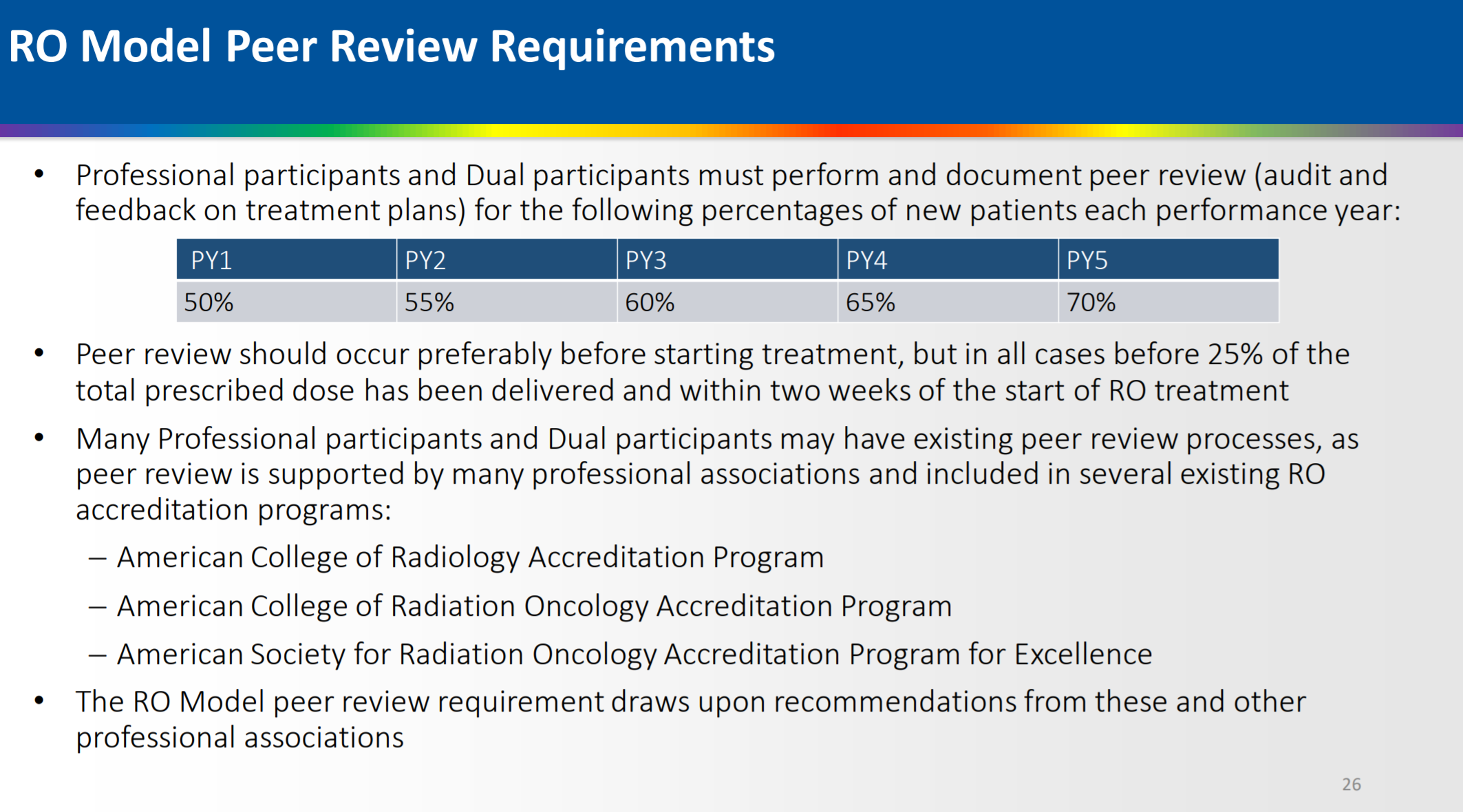
To facilitate safer RT delivery, the RO Model will also require adherence to nationally recognized, evidence-based clinical treatment guidelines when appropriate; peer review of treatment plans in all cases before 25% of the total prescribed dose has been delivered
What in the actual ****? Is there literally any other physician that has to run their care past a colleague. We all have to do it, for every patient? Imagine telling a surgeon he/she can't operate until someone else gives the thumbs up. This is the most ridiculous thing I've ever seen and you can definitely tell that the PPS exempt docs on the board threw this in as a further obstacle for small community practices to climb.
What in the actual ****? Is there literally any other physician that has to run their care past a colleague. We all have to do it, for every patient? Imagine telling a surgeon he/she can't operate until someone else gives the thumbs up. This is the most ridiculous thing I've ever seen and you can definitely tell that the PPS exempt docs on the board threw this in as a further obstacle for small community practices to climb.
- Joined
- Nov 2, 2019
- Messages
- 3,495
- Reaction score
- 14,489
This is straight propaganda. The fact that they published this now, though, basically destroys my last shred of hope this would be delayed again.Straight from the horses mouth:
- Joined
- Apr 21, 2011
- Messages
- 3,620
- Reaction score
- 9,243
Protons included BTWThis is straight propaganda. The fact that they published this now, though, basically destroys my last shred of hope this would be delayed again.
- Joined
- Oct 4, 2017
- Messages
- 5,015
- Reaction score
- 9,781
I have nothing against pe
imagine telling a medonc, colleague has to review chemo plan?To facilitate safer RT delivery, the RO Model will also require adherence to nationally recognized, evidence-based clinical treatment guidelines when appropriate; peer review of treatment plans in all cases before 25% of the total prescribed dose has been delivered
What in the actual ****? Is there literally any other physician that has to run their care past a colleague. We all have to do it, for every patient? Imagine telling a surgeon he/she can't operate until someone else gives the thumbs up. This is the most ridiculous thing I've ever seen and you can definitely tell that the PPS exempt docs on the board threw this in as a further obstacle for small community practices to climb.
- Joined
- Apr 3, 2019
- Messages
- 4,263
- Reaction score
- 9,929
Guys, been warning you... it's bad, bad, bad. Join Luh warned us too. It starts at ~50% of all cases I believe, then moves up to all cases later years.To facilitate safer RT delivery, the RO Model will also require adherence to nationally recognized, evidence-based clinical treatment guidelines when appropriate; peer review of treatment plans in all cases before 25% of the total prescribed dose has been delivered
What in the actual ****? Is there literally any other physician that has to run their care past a colleague. We all have to do it, for every patient? Imagine telling a surgeon he/she can't operate until someone else gives the thumbs up. This is the most ridiculous thing I've ever seen and you can definitely tell that the PPS exempt docs on the board threw this in as a further obstacle for small community practices to climb.
Taken to a logical extreme, a solo rad onc (without a partner) can no longer bill Medicare for rad onc.
- Joined
- Jul 26, 2007
- Messages
- 12,692
- Reaction score
- 2,310
I have nothing against pe
imagine telling a medonc, colleague has to review chemo plan?
Sometimes I wish I could review my medoncs chemo plans. It could have saved me a few headaches down the road.
- Joined
- Apr 21, 2011
- Messages
- 3,620
- Reaction score
- 9,243
You have a great point about 8Gy x 1. Hard to peer review that before 25% is delivered. Maybe you pause at 200 MU given and chat with the gown delivery guy (who is qualified to supervise the treatment delivery, btw) or something.Guys, been warning you... it's bad, bad, bad. Join Luh warned us too. It starts at ~50% of all cases I believe, then moves up to all cases later years.
Taken to a logical extreme, a solo rad onc (without a partner) can no longer bill Medicare for rad onc.
- Joined
- Apr 3, 2019
- Messages
- 4,263
- Reaction score
- 9,929
When you are not a rad onc (ie a nurse at CMS) and you start layering rules and regulations over top rad onc you're going to get some straight up illogical and silly and head-scratching situations that make it almost impossible for you as the MD to accomplish what you would like to do without a wee bit of fraud occurring. This is like when kV Xray supervision rules required physicians to stand at the machine all day, except maybe 10 times as stupid IMHO.You have a great point about 8Gy x 1. Hard to peer review that before 25% is delivered. Maybe you pause at 200 MU given and chat with the gown delivery guy (who is qualified to supervise the treatment delivery, btw) or something.
- Joined
- Oct 10, 2011
- Messages
- 8,624
- Reaction score
- 10,696
Straight from the horses mouth:
Why the **** was this published in JCO? **** them and their editors for allowing this nonsense into the journal.
No discussion of the concerns that many have had about the issues with RO-APM. None whatsoever.
I suppose they have no incentive to actually address anyone concerns. I look forward to the dumpster fire this will be in the unfortunate zip codes chosen for this human experiment.
- Joined
- Apr 16, 2004
- Messages
- 4,661
- Reaction score
- 5,079
This will only be a major issue for small practices though, doesn't everyone have weekly chart rounds? Anyways, with the upcoming workforce surplus, we can simply hire a "QA consultant" newly graduating resident and pay them $80k -right? Also, we can have them answer phones and mop the floor during dead time.
- Joined
- Apr 28, 2005
- Messages
- 1,196
- Reaction score
- 3,433
Included modalities: External beam radiotherapy (3-dimensional conformal radiotherapy, intensity modulated radiotherapy, stereotactic radiosurgery, stereotactic body radiotherapy, and proton beam therapy [PBT]) and brachytherapy (please refer to the CY 2022 OPPS and ASC Payment System Notice of Proposed Rulemaking (CMS-1753-P) to see proposed revisions to the RO Model design."Protons included BTW
But then it says, "For PBT, a substantially costlier modality than other modalities, the clinical trial exception will continue to enable providers and suppliers to generate evidence about PBT, allowing innovation in this field to continue."
So as long as you put the patient on a registry protons will be exempted I guess?
- Joined
- Apr 28, 2005
- Messages
- 1,196
- Reaction score
- 3,433
And don't forget the real point of this whole exercise.Straight from the horses mouth:
"In addition to supporting financial predictability, collaboration, and performance improvement in the field of RO, we estimate the RO Model will reduce Medicare radiation therapy spending by approximately 3% if the proposals described in the CY 2022 OPPS and ASC Payment System Notice of Proposed Rulemaking (CMS-1753-P) are finalized."
- Joined
- Apr 3, 2019
- Messages
- 4,263
- Reaction score
- 9,929
Dear RO Participant,
You are receiving this email because you have contacted the Centers for Medicare & Medicaid Services (CMS) RO Model Help Desk or attended an RO Model event. In anticipation of the proposed RO Model start date of January 1, 2022, the RO Model Team is hosting the Clinical Data Elements and Quality Measures Reporting Requirements webinar and seeking RO participants’ input on future events.
UPCOMING EVENT!
Click here to register for the
Clinical Data Elements and Quality Measures Reporting Requirements webinar
The Clinical Data Elements and Quality Measures Reporting Requirements webinar will occur on November 16, 2021 from 3:00-4:30 p.m. ET. During this 90-minute event, the RO Model Team will:
· Detail clinical data elements (CDEs) and quality measures (QMs) included in the RO Model and submission requirements
· Provide guidance for submission of CDEs and QMs, including use of the RO Model Secure Data Portal
· Discuss the integration of data collection and reporting and electronic health record systems
· Explain the Aggregate Quality Score methodology, including pay-for-performance and pay-for-reporting, as it relates to the CDEs and QMs
· Answer RO participants’ questions about the CDEs and QMs reporting requirements
Reminder! QM and CDE reporting is only a requirement for Professional participants and Dual participants.
How to Join:
Click on the hyperlinked ‘click here’ above to access the registration page (https://mathematicaevents.webex.com/mathematicaevents/onstage/g.php?MTID=e0f4ae5c64c13af51112154258db5ff53), find the registration information on the RO Model website (https://innovation.cms.gov/innovation-models/radiation-oncology-model), or check out the Events section of RO Connect. RO participants are encouraged to register for the webinar by November 15, 2021. It is recommended that attendees use either Microsoft Edge or Google Chrome to join the event.
Who Should Attend?
These events are designed for RO participants, particularly Professional and Dual participants. This includes staff at participating physician group practices, freestanding radiation therapy centers, and hospital outpatient departments who are supporting their organization in participation in the RO Model. For instance, clinicians, practice or quality managers, administrative personnel, financial analysts, and executive leadership from RO participants.
Access to Post-event Materials:
The RO Model Team will post slides and a recording of the webinar a few days after the event on the RO Model website and in RO Connect (search term “clinical data elements and quality measures”). When available, the RO Model Team will also post a transcript for the webinar in RO Connect using the same search term.
The RO Model Team seeks RO participants' input on the best times to hold future learning events (e.g., webinars, office hours). Please complete the Day and Time Preferences for Learning Events survey by November 17, 2021 to help inform when the RO Model Team schedules future learning events. This survey should only take a few minutes to complete.
Access the survey:
Click on the hyperlinked ‘click here’ above or access the full link for the survey at https://www.surveymonkey.com/r/ROModel.
You are receiving this email because you have contacted the Centers for Medicare & Medicaid Services (CMS) RO Model Help Desk or attended an RO Model event. In anticipation of the proposed RO Model start date of January 1, 2022, the RO Model Team is hosting the Clinical Data Elements and Quality Measures Reporting Requirements webinar and seeking RO participants’ input on future events.
UPCOMING EVENT!
Click here to register for the
Clinical Data Elements and Quality Measures Reporting Requirements webinar
The Clinical Data Elements and Quality Measures Reporting Requirements webinar will occur on November 16, 2021 from 3:00-4:30 p.m. ET. During this 90-minute event, the RO Model Team will:
· Detail clinical data elements (CDEs) and quality measures (QMs) included in the RO Model and submission requirements
· Provide guidance for submission of CDEs and QMs, including use of the RO Model Secure Data Portal
· Discuss the integration of data collection and reporting and electronic health record systems
· Explain the Aggregate Quality Score methodology, including pay-for-performance and pay-for-reporting, as it relates to the CDEs and QMs
· Answer RO participants’ questions about the CDEs and QMs reporting requirements
Reminder! QM and CDE reporting is only a requirement for Professional participants and Dual participants.
How to Join:
Click on the hyperlinked ‘click here’ above to access the registration page (https://mathematicaevents.webex.com/mathematicaevents/onstage/g.php?MTID=e0f4ae5c64c13af51112154258db5ff53), find the registration information on the RO Model website (https://innovation.cms.gov/innovation-models/radiation-oncology-model), or check out the Events section of RO Connect. RO participants are encouraged to register for the webinar by November 15, 2021. It is recommended that attendees use either Microsoft Edge or Google Chrome to join the event.
Who Should Attend?
These events are designed for RO participants, particularly Professional and Dual participants. This includes staff at participating physician group practices, freestanding radiation therapy centers, and hospital outpatient departments who are supporting their organization in participation in the RO Model. For instance, clinicians, practice or quality managers, administrative personnel, financial analysts, and executive leadership from RO participants.
Access to Post-event Materials:
The RO Model Team will post slides and a recording of the webinar a few days after the event on the RO Model website and in RO Connect (search term “clinical data elements and quality measures”). When available, the RO Model Team will also post a transcript for the webinar in RO Connect using the same search term.
The RO Model Team seeks RO participants' input on the best times to hold future learning events (e.g., webinars, office hours). Please complete the Day and Time Preferences for Learning Events survey by November 17, 2021 to help inform when the RO Model Team schedules future learning events. This survey should only take a few minutes to complete.
Access the survey:
Click on the hyperlinked ‘click here’ above or access the full link for the survey at https://www.surveymonkey.com/r/ROModel.
- Joined
- Nov 2, 2019
- Messages
- 3,495
- Reaction score
- 14,489
Ah, there it is, the loophole for protons big enough to drive a truck through.Included modalities: External beam radiotherapy (3-dimensional conformal radiotherapy, intensity modulated radiotherapy, stereotactic radiosurgery, stereotactic body radiotherapy, and proton beam therapy [PBT]) and brachytherapy (please refer to the CY 2022 OPPS and ASC Payment System Notice of Proposed Rulemaking (CMS-1753-P) to see proposed revisions to the RO Model design."
But then it says, "For PBT, a substantially costlier modality than other modalities, the clinical trial exception will continue to enable providers and suppliers to generate evidence about PBT, allowing innovation in this field to continue."
So as long as you put the patient on a registry protons will be exempted I guess?
- Joined
- Apr 3, 2019
- Messages
- 4,263
- Reaction score
- 9,929
- Joined
- Sep 7, 2014
- Messages
- 3,206
- Reaction score
- 5,904
I have no access to second physician, but do chart rounds weekly with physics, dosi, and RTTs. Is this good enough? If not, hence the reason I started a separate thread about this. Presumably ASTRO will help us single site docs find a match/navigate any HIPPA issues...
- Joined
- Apr 21, 2011
- Messages
- 3,620
- Reaction score
- 9,243
If you're a med student considering this disaster of a field, run the **** away.
You can't even treat patients without an okay from someone else.
Most ****ing ridiculous thing I've ever seen.
You can't even treat patients without an okay from someone else.
Most ****ing ridiculous thing I've ever seen.
- Joined
- Sep 20, 2004
- Messages
- 11,734
- Reaction score
- 11,827
Apparently oral boards and ongoing MOC which costs us real time and $$$ is for $h!t$ and gigglesIf you're a med student considering this disaster of a field, run the **** away.
You can't even treat patients without an okay from someone else.
Most ****ing ridiculous thing I've ever seen.
- Joined
- Nov 2, 2019
- Messages
- 3,495
- Reaction score
- 14,489
Coming soon: Elementary Chart Rounds, PLLCI have no access to second physician, but do chart rounds weekly with physics, dosi, and RTTs. Is this good enough? If not, hence the reason I started a separate thread about this. Presumably ASTRO will help us single site docs find a match/navigate any HIPPA issues...
I will meet with your department via Zoom as a second physician in chart rounds to comply with APM requirements. You may think my fees are steep, but can you really put a price on keeping your doors open?
- Joined
- Apr 21, 2011
- Messages
- 3,620
- Reaction score
- 9,243
Exactly! Why have a boarding process at all? It's a group think, hive mind specialty apparently.Apparently oral boards and ongoing MOC which costs us real time and $$$ is for $h!t$ and giggles
This is definitely put in there solely to disrupt/spite small practices.
- Joined
- Apr 21, 2011
- Messages
- 3,620
- Reaction score
- 9,243
To be fair: It does say, "when possible" "include physicians". I do a weekly chart rounds with my physics, dosi, RTTs, RN, OPNs, SLP, OT/PT, etc... Does that count?
- Joined
- Apr 3, 2019
- Messages
- 4,263
- Reaction score
- 9,929
I think it would. A "peer" is not (yet) defined by Medicare to be an MD. An ACGME board certified physicist... I certainly consider he/she a peer.To be fair: It does say, "when possible" "include physicians". I do a weekly chart rounds with my physics, dosi, RTTs, RN, OPNs, SLP, OT/PT, etc... Does that count?
- Joined
- Mar 20, 2013
- Messages
- 1,912
- Reaction score
- 3,506
Included modalities: External beam radiotherapy (3-dimensional conformal radiotherapy, intensity modulated radiotherapy, stereotactic radiosurgery, stereotactic body radiotherapy, and proton beam therapy [PBT]) and brachytherapy (please refer to the CY 2022 OPPS and ASC Payment System Notice of Proposed Rulemaking (CMS-1753-P) to see proposed revisions to the RO Model design."
But then it says, "For PBT, a substantially costlier modality than other modalities, the clinical trial exception will continue to enable providers and suppliers to generate evidence about PBT, allowing innovation in this field to continue."
So as long as you put the patient on a registry protons will be exempted I guess?
This is the first I’ve heard of this. Looks like you’re correct but can anyone else chime in?
Is registry enough ? Or does it have to be higher phase trial?
If it’s just registry then for all practical purposes you e got a proton carve out.
- Joined
- Aug 23, 2014
- Messages
- 3,265
- Reaction score
- 6,618
Lots of chit chat about a proton excemption being carved out, heavily advocated for behind closed doors. WOW it looks like it is actually happening?
The chart round requiremend starts at 50 pct and increases eventually to 100 i think
The chart round requiremend starts at 50 pct and increases eventually to 100 i think
- Joined
- Sep 20, 2004
- Messages
- 11,734
- Reaction score
- 11,827
Swamp is alive and well at astro and CMSLots of chit chat about a proton excemption being carved out, heavily advocated for behind closed doors. WOW it looks like it is actually happening?
The chart round requiremend starts at 50 pct and increases eventually to 100 i think
How does a solo practioner do "peer-review" for a sim-and-treat 8 Gy x 1?
- Joined
- Oct 4, 2017
- Messages
- 5,015
- Reaction score
- 9,781
Lots of chit chat about a proton excemption being carved out, heavily advocated for behind closed doors. WOW it looks like it is actually happening?
The chart round requiremend starts at 50 pct and increases eventually to 100 i think
Really sick. Residency expansion, Instructorships, and now proton exemption. That’s why I asked about what POS would deliver ASTROs “masterclass in leadership.”Swamp is alive and well at astro and CMS
- Joined
- Apr 3, 2019
- Messages
- 4,263
- Reaction score
- 9,929
You 1) do not, or 2) as @Mandelin Rain suggested, you stop the fraction delivery at 2 Gy, and chat with someone about the treatment, and then turn the beam back on. Other treatments such as single fx SBRT for oligomets will be similarly affected.How does a solo practioner do "peer-review" for a sim-and-treat 8 Gy x 1?
- Joined
- Apr 3, 2019
- Messages
- 4,263
- Reaction score
- 9,929
Protons exempt. Essentially. Hate to say I told you so. Nah... I told you so.
Similar threads
- Replies
- 78
- Views
- 3K
- Replies
- 451
- Views
- 24K