- Joined
- Oct 5, 2015
- Messages
- 2,882
- Reaction score
- 3,263
- Points
- 5,286
- Psychologist
Unnecessary. Baldur's Gate 3 is out.Did you post the link to Wizards of the Coast (publishers of Dungeons & Dragons)?

Unnecessary. Baldur's Gate 3 is out.Did you post the link to Wizards of the Coast (publishers of Dungeons & Dragons)?
I'm a 1st edition (AD&D) man myself.Unnecessary. Baldur's Gate 3 is out.
Did you post the link to Wizards of the Coast (publishers of Dungeons & Dragons)?
Unnecessary. Baldur's Gate 3 is out.
Sorry, 2nd edition all the way.I'm a 1st edition (AD&D) man myself.
We should create APA Division 57: The Division of Woo
Did you walk uphill both ways to get your handbook, Grandpa?I'm a 1st edition (AD&D) man myself.
Agreed. THAC0 for life.Sorry, 2nd edition all the way.
Ordered it by mail order through Sears & Roebuck (and we LIKED it!!!)Did you walk uphill both ways to get your handbook, Grandpa?
2nd edition, especially rulebooks, were MUCH more coherently put together.Sorry, 2nd edition all the way.
I think we might've tried once or twice just to see how it was and then we gave up. The books were much shorter, though, I'll give them that. And the hand-drawn art was...unique. Pretty sure I still have a 1e Dungeon Master's Guide lying around somewhere. And I know I have a whole bunch of 2e books in a closet.2nd edition, especially rulebooks, were MUCH more coherently put together.
And 1e combat rules (as written)...ugh...nobody I know actually ran them exactly as written.
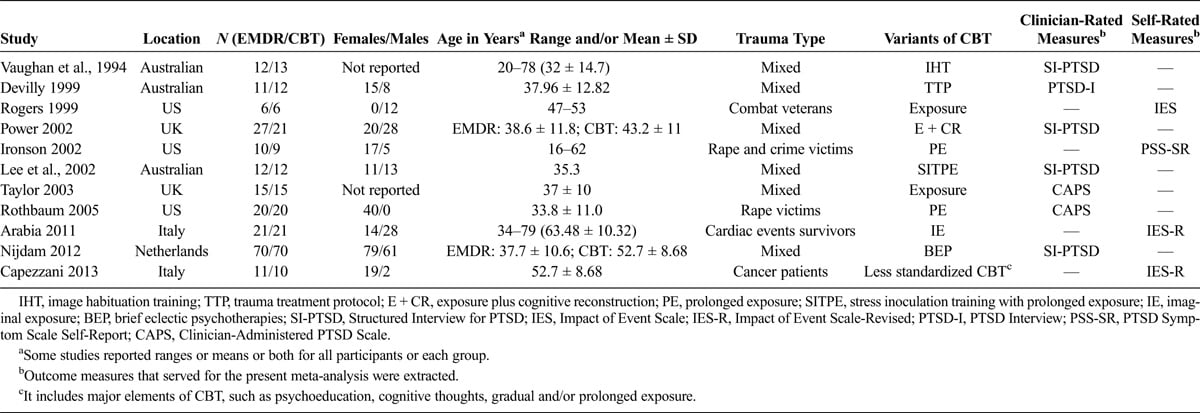
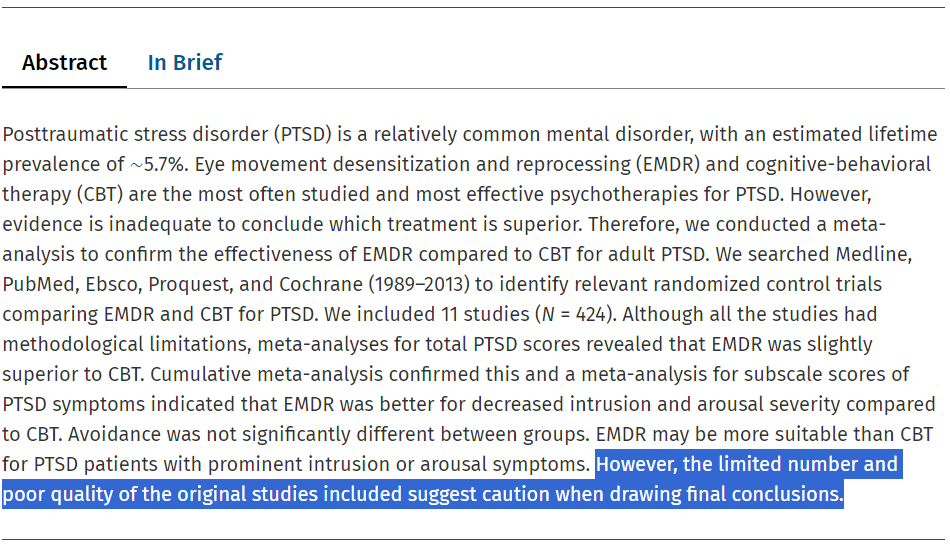
As you mentioned, EMDR IS effective. That's why it's recommended as a top tier therapy even by the DoD/VA PTSD guidelines. The problem isn't so much "does EMDR work?" but "how does EMDR work?" or "does EMDR work better than PE or CPT?" Regarding the latter question, supposedly Shapiro refused to do comparison studies with PE or CPT, but that research is now being done and will be forthcoming. From what I've heard, it sounds like EMDR works as well but doesn't have as lasting effects.

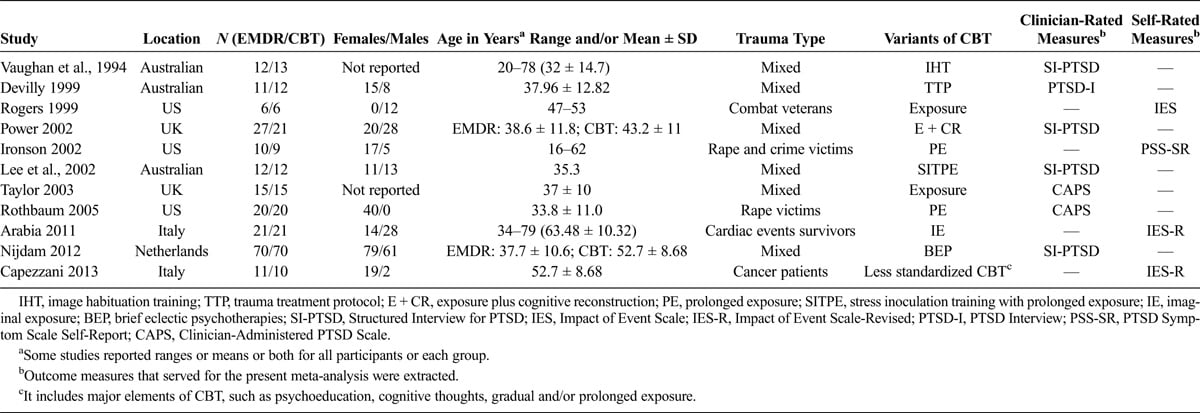

Plenty of research has been done comparing CBT or PE to EMDR.
Much of the research shows that there is no significant difference between the three therapies.
EMDRA placebo pill is not the cure to cancer. It is not a miracle treatment, regardless of the assertions of Oprah, Sandra Bullock or Prince Harry.
Does exposure therapy work faster when combined with a placebo pillEMDR? Maybe.
Worst-case scenario - You wore a purple hat. Nobody noticed.
Best-case scenario - Your client achieved their goals faster.
Most-likely scenario - Your client is happy that you use a placebo pillstrobe lights. You are happy that your client is happy. You get more referrals.
Cue the firing squad.
There's also some evidence (albeit weak) that EMDR increases likelihood of spontaneous false recall (an effect I'd imagine is particularly strong in individuals with high levels of suggestibility):
So yeah, I don't agree that "at worst, you wore a purple hat." No, at worst, you walk away with false memories and a false interpretive framework by which to understand your recovery process. I just don't get it--the supposed neurological mechanisms underlying EMDR have been debunked time and again, and then the acolytes move to some other speculative mechanism, endlessly moving the goalposts. If they'd just accept that it's simply an indirect, imaginal exposure therapy and strip all the BS from it then far fewer folks would have academic and ethical issues with it. It's not okay to lie to patients in clinical settings.
At the end of the day, it is all about the marketing. Why just be another practitioner of CBT, PE, or CPT when you can be the "expert" in EMDR. I see a lot or midlevels marketing their expertise because a lot of doctoral level providers don't offer it. Comes down to the $$$.
I'd argue that it's all the cases with EMDR. Either they're extolling the pseudo-neuroscience virtues out of ignorance or they know it's bunk and are intentionally deceiving patients.And in many cases, willful ignorance, or downright intentional malfeasance.
They (including our local evidence-based coordinator person) were heavily pushing everyone to get EMDR training/certification about a year ago. Glad I didn't take them up on it. The one rule I absolutely have for patients is that I do not lie to my patients (surprisingly hard to follow in the VA system sometimes). I would have hated to have to 'nope' my way out as soon as I learned about the pseudoscientific foundations and then have that 'mark' against me (every time you apply for training in an EBP protocol, they ask if you've ever dropped out of a training before).I'd argue that it's all the cases with EMDR. Either they're extolling the pseudo-neuroscience virtues out of ignorance or they know it's bunk and are intentionally deceiving patients.
They (including our local evidence-based coordinator person) were heavily pushing everyone to get EMDR training/certification about a year ago. Glad I didn't take them up on it. The one rule I absolutely have for patients is that I do not lie to my patients (surprisingly hard to follow in the VA system sometimes). I would have hated to have to 'nope' my way out as soon as I learned about the pseudoscientific foundations and then have that 'mark' against me (every time you apply for training in an EBP protocol, they ask if you've ever dropped out of a training before).
First session, I always ask my patients for honesty because we don't make progress without it. The least I can do is model the same for them.
But, I mean, what if by lying to them, I'm "helping" them, and by extension, helping myself to their money through dishonest means?
/s
This got three likes. Apparently, people with PHDs aren't sufficiently trained to READ. I'll narrow this down for you so you don't, heaven forfend, have to read all of the articles I quoted earlier.There aren't any RCTs comparing them, though. That's what I meant.

This is honest and correct. EMDR practitioners use odious marketing, loads of pseudoneurojargon to sell the product and, worst of all, apply EMDR to cases where it has no empirical basis whatsoever.I don't know many people who dispute the fact that EMDR shows some effectiveness, driven by the exposure component. I believe that the major contention lies in the fact that if we believe in informed consent, some providers are straight out lying to patients about the treatment as it relates to the useless components. As in, when discussing the treatment and mechanisms of action, they are spouting off pseudoneurojargon that has no basis in reality to get the patient to buy in. This is the odious part of the treatment.
Pair that with the fact that many of the EMDR cult are quite vocal in the "harm"that other trauma treatments cause while spouting off their nonsense. Pair that again with the fact that EMDR is increasingly marketed to target things like substance use, obesity, eating disorders, schizophrenia, among other things, thins for which little, if any empirical support exists. EMDR is unquestioningly a negative influence within the field.
Weak is an understatement. After declaring their bias against EMDR (In case you haven't noticed having a PHD would've been enough to tell us this) the authors themselves are totally inconclusive about their findings on every level.There's also some evidence (albeit weak) that EMDR increases likelihood of spontaneous false recall (an effect I'd imagine is particularly strong in individuals with high levels of suggestibility):
So yeah, I don't agree that "at worst, you wore a purple hat." No, at worst, you walk away with false memories and a false interpretive framework by which to understand your recovery process. I just don't get it--the supposed neurological mechanisms underlying EMDR have been debunked time and again, and then the acolytes move to some other speculative mechanism, endlessly moving the goalposts. If they'd just accept that it's simply an indirect, imaginal exposure therapy and strip all the BS from it then far fewer folks would have academic and ethical issues with it. It's not okay to lie to patients in clinical settings.
…Apparently, people with PHDs aren't sufficiently trained to READ. I'll narrow this down for you so you don't, heaven forfend, have to read all of the articles I quoted earlier.
Did you read those articles?This got three likes. Apparently, people with PHDs aren't sufficiently trained to READ. I'll narrow this down for you so you don't, heaven forfend, have to read all of the articles I quoted earlier.

Effectiveness of EMDR for decreasing symptoms of over‐arousal: A meta‐analysis
A meta-analysis was conducted to evaluate the comparative effectiveness of eye movement desensitization and reprocessing (EMDR) in the treatment of symptoms of over-arousal and comparing effectivenes...onlinelibrary.wiley.com
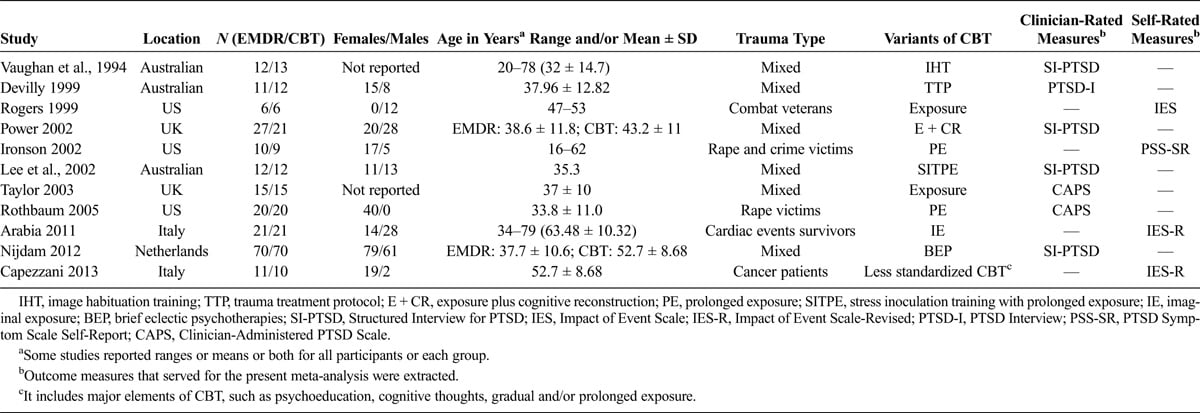
Eye Movement Desensitization and Reprocessing Versus... : The Journal of Nervous and Mental Disease
evidence is inadequate to conclude which treatment is superior. Therefore, we conducted a meta-analysis to confirm the effectiveness of EMDR compared to CBT for adult PTSD. We searched Medline, PubMed, Ebsco, Proquest, and Cochrane (1989–2013) to identify relevant randomized control trials...journals.lww.com
If you kept reading and didn't read at least the damned abstracts of those three studies, go return your Phd. The world will be a better place.
There have been dismantling studies which tell us why EMDR "works," and it's not the things that are unique to EMDR, i.e., the pseudo-neuroscience.This is honest and correct. EMDR practitioners use odious marketing, loads of pseudoneurojargon to sell the product and, worst of all, apply EMDR to cases where it has no empirical basis whatsoever.
The EMDR culture is terrible for the field.
But y'all are scientists - so leave aside the culture and let's talk about the actual treatment.
- It has no know mechanism of action. That's fine. Neither does lithium or Tylenol. Nobody could care less. If it works.
Wow, you're being so neutral and very much not steering your patient into one particular treatment over the other, huh?- Ethical problems. I have you covered.
I'd like to tell my client - "Listen there is this experimental treatment involving these here strobe lights - nobody has a clue how it works, but some studies have shown that it may help you get better faster with less homework. Those studies are definitely not conclusive, experimental at best, but if you're interested we could try it. Would you like to try that or should I send home these here CBT worksheets with you?"
Any ethical problem with that?
Who here has said anything about the "association" or allowing that to cause you to not help patients?I get it. The EMDR culture is full of ethical issues. Agreed. But just because those practitioners tend to be dumb as a doorknob and as honest as a snake that doesn't mean that you should dismiss the efficacy of the treatment out of hand without giving it an academic chance.
You know what I do have an ethical problem with?
Not doing what may help your client because it would make you look bad by association.
What?"ME?! The great and holy scientific mind?! I would never be caught dead doing anything that would associate me with those plebian EMDR folk."
Because there are evidence-based interventions that aren't "experimental" and don't rely on deceiving patients about them to various degrees.Honestly, I do want to know if anyone has a a good reason why not to take the limited findings supporting EMDR for exactly what they are and to present them to clients as such - an experimental procedure with no known mechanism-of-action that may help them, if they want it.
When you have to compare criticism of your intervention with turning off a lamp, you're definitely arguing in good-faith.Especially if for some reason they are dead-set on it - why refuse to provide something that will make your client happy as long as you are being perfectly honest about what it is? Your client asks you to turn off that extra lamp because they prefer it was a little darker... "I'm sorry, there isn't sufficient empirical basis to justify modifying the lumen-exposure-rate in the context of this therapeutical intervention." Just turn off the lamp.
Your client is a person. Do whatever it takes to make them feel comfortable and help them achieve their goals. That is the highest ethical standard I know.
Any thoughts?
You left out the part that concludes that while there is little evidence that EMDR increases susceptibility to misinformation (i.e., taking on information fed to you by someone else), there is evidence that the eye movements "...do seem to increase spontaneous false memories" (i.e., recall that is erroneous and not related to information being directly fed to you; emphasis mine). This is a literature review of a small number of papers. No one is calling it perfect, but the methods are good for the data they have, and it directly contradicts the claim that EMDR is, at worst, a purple hat therapy. Again, I outright said the evidence is weak...but it does exist and would imply potential for iatrogenic harm.Weak is an understatement. After declaring their bias against EMDR (In case you haven't noticed having a PHD would've been enough to tell us this) the authors themselves are totally inconclusive about their findings on every level.
From the article's Final Remarks:
"We do not have strong evidence that EM affect susceptibility to misinformation one way or another. That is, the EM involved in EMDR do not appear to consistently enhance memory, nor do they appear to consistently increase misinformation endorsement."
I will leave it at that and not discuss the myriad methodological issues with that article.
It does have a known mechanism of action. Exposure. Oh, and Tylenol inhibits COX-1 and COX-2. You're right about lithium, but, again, lithium's mechanism is truly unknown. EMDR's is not. Dismantling studies have demonstrated, time and time and time and time again, that bilateral stimulation is not a differentially efficacious component--it does not enhance the treatment in any measurable way.- It has no know mechanism of action. That's fine. Neither does lithium or Tylenol. Nobody could care less. If it works.
(a) We do know how EMDR works and that it works via the same common mechanisms that make everything else work (i.e., exposure, meaning-making, re-appraisal).- Ethical problems. I have you covered.
I'd like to tell my client - "Listen there is this experimental treatment involving these here strobe lights - nobody has a clue how it works, but some studies have shown that it may help you get better faster with less homework. Those studies are definitely not conclusive, experimental at best, but if you're interested we could try it. Would you like to try that or should I send home these here CBT worksheets with you?"
This is why all doctoral-level graduate students should receive formal training in the philosophy of science.Did you read those articles?
View attachment 383521View attachment 383522
There have been dismantling studies which tell us why EMDR "works," and it's not the things that are unique to EMDR, i.e., the pseudo-neuroscience.
Wow, you're being so neutral and very much not steering your patient into one particular treatment over the other, huh?
Couching something as "experimental" doesn't excuse you for deceiving patients about what the literature actually is or being oh-so-subtle in how you frame it versus other treatments.
Who here has said anything about the "association" or allowing that to cause you to not help patients?
What I've seen is people recommending other evidence-based treatments for trauma like CPT and PE.
What?
Because there are evidence-based interventions that aren't "experimental" and don't rely on deceiving patients about them to various degrees.
When you have to compare criticism of your intervention with turning off a lamp, you're definitely arguing in good-faith.
There's lots of things that would make patients feel more comfortable. There's also lots of things that they want or think would make them happy. They'd probably feel better and happier if every session came with complimentary steak and lobster.
There's no ethical obligation or standard to give patients everything they want or to give them the intervention that they are demanding. Patient preferences are important, but they're just that, preferences. This is a gross misunderstanding of our ethical obligations and evidence-based practice.
100% agreed, though most of my training in this was in undergrad. Philosophy of science were probably my favorite courses in undergrad.This is why all doctoral-level graduate students should receive formal training in the philosophy of science.
This is why I'm so irked by this kind of pseudoscience, but also things like DID.Characteristics of good theories:
independently testable: An auxiliary hypothesis must be testable independently of the theory it was is introduced to save.
unified: It should be simple and have a small number of problem solving strategies that can be applied to a large number of situations.
fecundity. A good theory should open up new areas of research.
A good theory should be as concerned with giving good explanations of unexplained phenomena as it is with generating correct predictions.
A good theoretical foundation for a psychological intervention must be consistent with the corpus of the entirety of the basic science upon which it is founded as well as all of the other sciences (biology, chemistry, evolutionary theory, areas of psychology (e.g., how memory works)).
Sounds like she was trying to mimic Marsha Linehan's backstory.About a decade or so ago I bought Francine Shapiro's EMDR text but I couldn't make it more than a few pages into it due to the anecdotal nature of the report of 'her discovery' involving her walking down a road and noticing that as she moved her eyes side to side randomly it relieved her psychological distress related to (I assume) traumatic memories. So, in the history of humankind, this potent 'effect'/discovery never took place until Francine Shapiro noticed it. Once I made it past that anecdote, I couldn't make it through the pseudoneurological 'scientisty'-sounding neuro-babble 'explanations' offered in the first chapter of that book regarding proposed mechanism of action.
And we don't have to be deceptive about it.To each his/her own, I suppose. When I share cognitive-behavioral explanations of clinical phenomena, I know that they rest on (admittedly imperfect) empirical literature that I can understand and meaningfully articulate. I'll stick to that.
Did you read those articles?
Obviously, this is the point we are trying to debate. Restating your opinion is hardly a refutation.There have been dismantling studies which tell us why EMDR "works," and it's not the things that are unique to EMDR, i.e., the pseudo-neuroscience.
I'm simply mentioning to you the reason why the client may prefer EMDR. People hate homework, and they like when they have to pay for less sessions of therapy.Wow, you're being so neutral and very much not steering your patient into one particular treatment over the other, huh?
I have been waiting patiently here for someone to explain to me why the evidence quoted is so terribly insufficient that it cannot be classified as an experimental enhancement to exposure therapy.Couching something as "experimental" doesn't excuse you for deceiving patients about what the literature actually is or being oh-so-subtle in how you frame it versus other treatments.
Who here has said anything about the "association" or allowing that to cause you to not help patients?
Spelling correction noted. I assume that your razor-sharp wit has not been distracted from the topic at hand.What I've seen is people recommending other evidence-based treatments for trauma like CPT and PE.
Plebian
What?
As noted ad nauseum, EMDR is always just an enhancement to a therapy that is evidence-based. There is no need to deceive patients about EMDR. It is an enhancement that has some very inconclusive backing that shows it may be helpful.Because there are evidence-based interventions that aren't "experimental" and don't rely on deceiving patients about them to various degrees.
When you have to take shots at an argument by attacking its illustrations instead of discussing the point, you're definitely arguing in good faith.When you have to compare criticism of your intervention with turning off a lamp, you're definitely arguing in good-faith.
It is not the clinicians job to provide food. It is his responsibility to provide the best care they can as a therapist. I do think that it is the clinician's responsibility to use a method that is less stressful and quicker if one is available. It is unethical to engage in a mode of therapy which will cause undue stress and lengthen the therapy process simply because you prefer it.There's lots of things that would make patients feel more comfortable. There's also lots of things that they want or think would make them happy. They'd probably feel better and happier if every session came with complimentary steak and lobster.
There's no ethical obligation or standard to give patients everything they want or to give them the intervention that they are demanding. Patient preferences are important, but they're just that, preferences. This is a gross misunderstanding of our ethical obligations and evidence-based practice.
You left out the part that concludes that while there is little evidence that EMDR increases susceptibility to misinformation (i.e., taking on information fed to you by someone else), there is evidence that the eye movements "...do seem to increase spontaneous false memories" (i.e., recall that is erroneous and not related to information being directly fed to you; emphasis mine). This is a literature review of a small number of papers. No one is calling it perfect, but the methods are good for the data they have, and it directly contradicts the claim that EMDR is, at worst, a purple hat therapy. Again, I outright said the evidence is weak...but it does exist and would imply potential for iatrogenic harm.
Obviously, this is the point we are trying to debate. Restating your opinion is hardly a refutation. Had to repeat that here. Sorry guys, I'm bored too. Love the confidence, though.It does have a known mechanism of action. Exposure. Oh, and Tylenol inhibits COX-1 and COX-2. You're right about lithium, but, again, lithium's mechanism is truly unknown. EMDR's is not. Dismantling studies have demonstrated, time and time and time and time again, that bilateral stimulation is not a differentially efficacious component--it does not enhance the treatment in any measurable way.
(a) We do know how EMDR works and that it works via the same common mechanisms that makes everything else work (i.e., exposure, meaning-making, re-appraisal).
Luckily the efficacy of CBT is not up for debate now, so you won't mind if I had some fun with it. Don't take it personally, please.(b) This is a complete strawman of CBT.
This is why all doctoral-level graduate students should receive formal training in the philosophy of science.
Characteristics of good theories:
independently testable: An auxiliary hypothesis must be testable independently of the theory it was is introduced to save.
unified: It should be simple and have a small number of problem solving strategies that can be applied to a large number of situations.
fecundity. A good theory should open up new areas of research.
A good theory should be as concerned with giving good explanations of unexplained phenomena as it is with generating correct predictions.
A good theoretical foundation for a psychological intervention must be consistent with the corpus of the entirety of the basic science upon which it is founded as well as all of the other sciences (biology, chemistry, evolutionary theory, areas of psychology (e.g., how memory works)).
About a decade or so ago I bought Francine Shapiro's EMDR text but I couldn't make it more than a few pages into it due to the anecdotal nature of the report of 'her discovery' involving her walking down a road and noticing that as she moved her eyes side to side randomly it relieved her psychological distress related to (I assume) traumatic memories. So, in the history of humankind, this potent 'effect'/discovery never took place until Francine Shapiro noticed it. Once I made it past that anecdote, I couldn't make it through the pseudoneurological 'scientisty'-sounding neuro-babble 'explanations' offered in the first chapter of that book regarding proposed mechanism of action.
To each his/her own, I suppose. When I share cognitive-behavioral explanations of clinical phenomena, I know that they rest on (admittedly imperfect) empirical literature that I can understand and meaningfully articulate. I'll stick to that.
Thank you.Interesting topic and a (mostly) civil discourse. Thus, this is a gentle reminder that personal attacks are not part of healthy discourse and may result in removal from the discussion (or the community).
Considering the sordid history of psychotherapy as it pertains to false recall, and considering the potential for effects demonstrated in a very carefully controlled environment to be amplified when used in uncontrolled clinical settings (potentially with folks who already have high memory biases and trait suggestibility), this could absolutely be a huge deal.Indeed I did. Perhaps I was wrong to think it obvious that there is no danger implied by a study that showed that people using EM gave more false positives when asked to identify words they had been shown in a word list.
You're the one who seems to think BLS does matter, so really it would be upon the claimants (those who claim BLS matters) to provide the evidence. However, since studies do exist:Waiting for the low-down on all of the dismantling studies (that's what I came here to hear). Thanks in advance. Really.
Okay, but you used that straw man as a legitimate argument in favor of using EMDR instead of "doing some worksheets." The snark is fine, but at least make it accurate.Luckily the efficacy of CBT is not up for debate now, so you won't mind if I had some fun with it. Don't take it personally, please.
No one was trying to debate anything until you hopped in and starting "playing the Devil's advocate." We were simply expressing our frustrations over APA--an ostensibly scientific organization--being wishy-washy in its actual advocacy for science-based treatment. We never asked for a debate.Obviously, this is the point we are trying to debate.
But it doesn't "enhance" anything.As noted ad nauseum, EMDR is always just an enhancement
Yes, again, because this topic has been rehashed for decades and this thread was not meant to be a replacement for a literature review.Apparently it's so clear to everyone else here that EMDR is bunk, that nobody has been bothered to bring the evidence
Would this be a good summary?
EMDR does not appear to have greater effectiveness than CPT, etc. (and may be less effective), there is some indication that it has increased risks of harm, but some patients may engage with it better than with CPT, etc.. The BLS might have utility in decreasing the intensity of the experience and as such have benefit, but it that utility is not greater than any other given effective distractor and the belief (and espousement thereof) in a special significance or mechanism to BLS (over other distractors) is significantly harmful.
As such, the EMDR modality may be appropriate in select patients so long as it includes a full disclosure of the evidence base and function of BLS in the treatment (perhaps ideally with a similar approach but different distractor) as well as possible risks of false memory.
Maybe this was already mentioned, but EMDR also doesn't really pass Safe, Easy, Cheap, and Sensible (SECS) sniff test given that's it's difficult to access, expensive to train in, and other treatments that are arguably more effective (in that they at least pose fewer risks) are readily available.
EMDR is just the biggest MLM scheme of the psychology world at the moment.
IFS is coming up in the rearviewEMDR is just the biggest MLM scheme of the psychology world at the moment.
I was just coming here to make this comparison. I have a problem with exploitative systems. Even if I decide to practice EMDR with a thorough informed consent outlining the evidence based vs non evidence based aspects, there is still the matter of the expense of training compared to other options. I would be shelling out money towards this system.EMDR is just the biggest MLM scheme of the psychology world at the moment.
IFS is coming up in the rearview
In the opinion of the psychologists here are there any interventions that are evidence-based besides CBT and exposure therapy?IFS is coming up in the rearview
The only definition of 'evidence-based psychotherapy' I've ever seen in print (or articulated anywhere) parallels the definition of 'evidence-based medicine' and it is, essentially, the intersection of:In the opinion of the psychologists here are there any interventions that are evidence-based besides CBT and exposure therapy?

 www.apa.org
www.apa.org
What are you trying to achieve by continually stirring the pot?In the opinion of the psychologists here are there any interventions that are evidence-based besides CBT and exposure therapy?
I may have mentioned before that I'm trying to learn some things from you guys. I mean that seriously.What are you trying to achieve by continually stirring the pot?
Yes, there are evidence-based theories that aren’t CBT or exposure therapy. IFS ain’t one of ‘em.
Unless you can start demonstrating the existence of “parts” and giving mechanistic evidence for achieving symptom reduction by reducing conflicts between these nebulous and unfalsifiable entities, then you’re not on strong footing.
So let me rephrase. Since coming here I've discovered that the APA is not the greatest source for information on EBPs. If anyone could share some practices that are evidence-based besides CBT, I would be eternally grateful.
What are they? Where could I find reliable information about them?
I dunno...honestly, I think that their publicly announced position on the definition (tri-partite) of 'evidence-based therapy' is one of the few things recently that APA has 'gotten right.'I may have mentioned before that I'm trying to learn some things from you guys. I mean that seriously.
I prefer when people explain things and substantiate their claims since it's otherwise difficult for me to accept their opinions as fact (which I hope you consider a merit). I appreciated FanMeehls post for example. It gave me a lot of information explaining what I hadn't understood beforehand.
I am not trying to piss anyone off. I'm just trying to get a helpful answers to questions that typically get canceled instead of answered.
I only stir the pot because people here sometimes assume you must be brain-dead to even have a question regarding certain things. That pretty much precludes me getting any useful answer to the question that I asked since it hasn't been taken seriously. After stirring the pot I got a lot of excellent substantive responses, including your own. A bit snide perhaps, but worth it anyway.
Regardless, no one is obligated to help me out. I simply appreciate it. My clients will appreciate it as well, as I'll be a better therapist.
(I bumped this particular thread instead of creating a new one because the OP expressed confusion that is similar to my own)
Just trying to figure things out here.
So let me rephrase. Since coming here I've discovered that the APA is not the greatest source for information on EBPs. If anyone could share some practices that are evidence-based besides CBT, I would be eternally grateful.
What are they? Where could I find reliable information about them?
(I understand, FanMeehl, that this question is not in line with the movement away from the "protocol-for-syndrome" approach. I think the answers would prove valuable to me regardless until I manage to achieve the expertise necessary for the approach mentioned in the article you quoted.)
Thank you all!
