Noticing a lot of people saying “rural jobs will always be available and have a shortage!” But im not really seeing this play out on the job boards. Yes, the only available jobs right now are rural, but shortage? Every day on practicelink the number of jobs continues to go down. How can we say with a straight face there will always be a shortage in these areas when fresh residents literally have no where else to go? There’s already way less than any other specialty on a job:resident ratio INCLUDING the supposedly endless rural jobs!
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
The rural job myth
- Thread starter skougess
- Start date
- Joined
- Sep 16, 2010
- Messages
- 1,295
- Reaction score
- 2,174
Sorry you're having a tough time with the job search. The market is terrible right now.
But...who on this forum has been painting the short-term outlook of EM with the rainbow and unicorn happy-time brush?
I think the general sentiment is that rural EM jobs are more available than urban jobs. Period.
While the EM job scene is bad, you may consider not using practicelink as a yardstick for the job market. From what I've heard it's more cumbersome and expensive than putting up ads on the many other online job boards. And the hospital-employed gigs, academic shops, and CMGs often post their jobs on their own websites--make sure you're checking their sites too. And don't be afraid to cold-call/email as many places simply don't advertise.
And, for what it's worth, practicing EM in rural spots can be awesome. The breadth of your skillset will be fully put to use (and it will grow), hospital admin/other docs will be happy you're there, and the patients are typically very grateful and unentitled. If my SO wouldn't divorce me, I'd gladly move back to the sticks.
But...who on this forum has been painting the short-term outlook of EM with the rainbow and unicorn happy-time brush?
I think the general sentiment is that rural EM jobs are more available than urban jobs. Period.
While the EM job scene is bad, you may consider not using practicelink as a yardstick for the job market. From what I've heard it's more cumbersome and expensive than putting up ads on the many other online job boards. And the hospital-employed gigs, academic shops, and CMGs often post their jobs on their own websites--make sure you're checking their sites too. And don't be afraid to cold-call/email as many places simply don't advertise.
And, for what it's worth, practicing EM in rural spots can be awesome. The breadth of your skillset will be fully put to use (and it will grow), hospital admin/other docs will be happy you're there, and the patients are typically very grateful and unentitled. If my SO wouldn't divorce me, I'd gladly move back to the sticks.
- Joined
- May 29, 2015
- Messages
- 2,402
- Reaction score
- 6,276
People say this because the people saying it have a nice cush urban/suburban job they've had forever and aren't looking.
If they spent even one second thinking about it, they'd realize it's not sustainable. We're all being pushed to rural spots now for jobs. It's only going to take 2-3 years at most (because residencies are still opening even this year) to fill all the rural spots with how many grads we have. Then what? I can't even imagine what people are going to be doing that are currently matching EM.
EM turnover is essentially non existent with being the youngest physician workforce and especially since the people with good jobs know this and are white knuckle gripping their jobs whereas in the past people moved freely.
I'm so sick of docs saying "I just got an email from (rural) wisconsin, there's plenty of jobs, just go there!". How about you older docs take these rural jobs instead.
Acep already recently just said that there is no job shortage and CMGs/PE aren't a problem so it's game over for any type of change
AAEM is the answer but they're too small and practicing docs don't care about new grads finding a job so they won't come together either.
rip
If they spent even one second thinking about it, they'd realize it's not sustainable. We're all being pushed to rural spots now for jobs. It's only going to take 2-3 years at most (because residencies are still opening even this year) to fill all the rural spots with how many grads we have. Then what? I can't even imagine what people are going to be doing that are currently matching EM.
EM turnover is essentially non existent with being the youngest physician workforce and especially since the people with good jobs know this and are white knuckle gripping their jobs whereas in the past people moved freely.
I'm so sick of docs saying "I just got an email from (rural) wisconsin, there's plenty of jobs, just go there!". How about you older docs take these rural jobs instead.
Acep already recently just said that there is no job shortage and CMGs/PE aren't a problem so it's game over for any type of change
AAEM is the answer but they're too small and practicing docs don't care about new grads finding a job so they won't come together either.
rip
- Joined
- Feb 22, 2014
- Messages
- 281
- Reaction score
- 189
Completely agree. When I graduated residency there was this idea that most ER docs leave their first job after 2-3 years. Nowadays, even if that job is solo coverage 100+ patients per day with envision or USACS, nobody is leaving.
I will say ACEP is holding some sort of "how to get a job in a pandemic" talk and I think they started or partnered with emcareers.org to give us a better job board. Not to say they aren't still a major problem, but it's something I guess?
I will say ACEP is holding some sort of "how to get a job in a pandemic" talk and I think they started or partnered with emcareers.org to give us a better job board. Not to say they aren't still a major problem, but it's something I guess?
Too many problems:
1) patient volumes down all around
2) no support from ACEP/ACGME, they do not care, their mission is more supply of healthcare “providers”
3) the future is single doc coverage with mid level support or mid level independent practice regardless of patient outcomes or increased health system expense
4) CMGs are too debt heavy and this downturn just accelerated what we all knew would happen once the PE money inflow stopped and PE looked for the exit $$$
5) We are losing the protection of our career because we are flooding the market with new grads (debt heavy) and replacements in the form of mid levels
Ultimately, I believe this will eliminate EM as a specialty because with these changes what is special about us?
1) patient volumes down all around
2) no support from ACEP/ACGME, they do not care, their mission is more supply of healthcare “providers”
3) the future is single doc coverage with mid level support or mid level independent practice regardless of patient outcomes or increased health system expense
4) CMGs are too debt heavy and this downturn just accelerated what we all knew would happen once the PE money inflow stopped and PE looked for the exit $$$
5) We are losing the protection of our career because we are flooding the market with new grads (debt heavy) and replacements in the form of mid levels
Ultimately, I believe this will eliminate EM as a specialty because with these changes what is special about us?
- Joined
- Jan 22, 2012
- Messages
- 858
- Reaction score
- 1,512
Step away from the ledge. Who/what do you think is going to replace EM? 100% mid-levels? Zero chance.Ultimately, I believe this will eliminate EM as a specialty because with these changes what is special about us?
- Joined
- Aug 21, 2007
- Messages
- 7,863
- Reaction score
- 13,576
Step away from the ledge. Who/what do you think is going to replace EM? 100% mid-levels? Zero chance.
He said it right in his post: single physician coverage with a crew of pretend-level-"providers", or the rural pretend-level-"provider" with some nebulous physician "oversight".
- Joined
- Feb 22, 2014
- Messages
- 281
- Reaction score
- 189
Was kind of reassuring to see that was written in 2011. But then I looked up the care providers at ellenville regional. I guess 1 doc for 7-8 midlevels is the future standard?
- Joined
- Sep 19, 2004
- Messages
- 2,950
- Reaction score
- 3,279
Was kind of reassuring to see that was written in 2011. But then I looked up the care providers at ellenville regional. I guess 1 doc for 7-8 midlevels is the future standard?
I have my doubts. This might work at some places, not others. At one of the hospitals I worked at, the ICU doc's group hired a bunch of midlevels, and tried to train them to intubate and place central lines. In one week, they had 3 patients with a pneumothorax, and one coded, which I had to attend to and place a chest tube, during a night shift. They also had major problems intubating easy airways with a glidescope. The CMO put an immediate stop to MLPs doing any of those procedures. You do this in a high acuity ED, there's going to be a lot of killing and maiming going on. Not saying it can't happen, but less likely.
- Joined
- Aug 21, 2007
- Messages
- 7,863
- Reaction score
- 13,576
I've said this before, but it bears repeating.
The only way for this PLP problem to be resolved is to give them the rope and let them tie their own noose.
Refuse to train them, refuse to supervise them, don't work for hospitals that do.
Let the attorneys feast on their incompetence, and let the public outcry be "we want to see the doctor".
Yeah, its going to be painful for us; but it will be worth it in the end.
We need to diversify ourselves in Birdstrike like fashion until then.
EDIT: Oh, and ACEP needs to be erased. Altogether.
The only way for this PLP problem to be resolved is to give them the rope and let them tie their own noose.
Refuse to train them, refuse to supervise them, don't work for hospitals that do.
Let the attorneys feast on their incompetence, and let the public outcry be "we want to see the doctor".
Yeah, its going to be painful for us; but it will be worth it in the end.
We need to diversify ourselves in Birdstrike like fashion until then.
EDIT: Oh, and ACEP needs to be erased. Altogether.
- Joined
- Jul 27, 2011
- Messages
- 2,255
- Reaction score
- 2,921
3 years ago as pgy3, the rural-ish jobs that were 1 hour from me were all open and needed moonlighters. All of them are fully staffed now. There are no rural jobs around me at least. Everything is tight. Im so glad i have a rural position locked down
- Joined
- Jan 22, 2012
- Messages
- 858
- Reaction score
- 1,512
He said it right in his post: single physician coverage with a crew of pretend-level-"providers", or the rural pretend-level-"provider" with some nebulous physician "oversight".
I guess to me that doesn't equate to the complete elimination of the specialty but YMMV.
- Joined
- Jan 22, 2012
- Messages
- 858
- Reaction score
- 1,512
Bob Donaldson is clinical director of emergency medicine and president of the medical staff at Ellenville Regional Hospital in New York. His current projects sound much like any medical staff president's goals.
What might surprise you is that Donaldson is not a physician but a nurse practitioner. He was elected to this influential position by his physician colleagues and enjoys great support from the hospital's medical staff.
I interviewed Donaldson to find out how a nurse practitioner broke down physician hierarchy and found an innovative hospital that could be a model for provider collegiality and meeting a community's healthcare needs.
"I passed muster, if you will, as the first non-physician, full-time, sole provider here as an NP working in the ER alongside the docs," he says. "It was so successful that we ultimately eliminated all the docs here and replaced them all with nurse practitioners or physician assistants.

Nurse Practitioner Elected Medical Staff President
A high-achieving nurse practitioner who was elected to the influential position of medical staff president with more than 50% of the all-physician vote explains his unusual rise through the ranks.www.healthleadersmedia.com
I find that hard to believe that will become the standard of care in US EDs. If a medical staff is that stupid then they got what they had coming.
- Joined
- Aug 21, 2007
- Messages
- 7,863
- Reaction score
- 13,576
I find that hard to believe that will become the standard of care in US EDs. If a medical staff is that stupid then they got what they had coming.
Its already happening, amigo.
- Joined
- Aug 21, 2007
- Messages
- 7,863
- Reaction score
- 13,576
I guess to me that doesn't equate to the complete elimination of the specialty but YMMV.
Close enough.
- Joined
- Jan 22, 2012
- Messages
- 858
- Reaction score
- 1,512
Its already happening, amigo.
Rural, yes. Urban, not even close.
- Joined
- Aug 21, 2007
- Messages
- 7,863
- Reaction score
- 13,576
Rural, yes. Urban, not even close.

15 Docs Fired From Illinois Health System to Be Replaced With NPs
A leaked internal memo says they will be replaced with advanced practice nurses as 'patients have made it very clear that they want less costly care and convenient access for lower-acuity issues.'
www.medscape.com
Happened at a few other shops that I know of. New CMG comes in, cuts staff and rates, replaces physicians with PLPs, forces those who remained to 'supervise' the PLPs.
- Joined
- Apr 27, 2014
- Messages
- 863
- Reaction score
- 1,501
Residency applicants usually ask me the same questions every year, but this year they routinely asked a new one: “Do advanced practice providers work in your emergency department?”
Some of this is driven by the revelation this past fall that several prominent universities with emergency medicine residencies also had emergency medicine “residencies” for physician assistants. The subsequent social media backlash was ugly, and anxiety is growing among EM residents and applicants about the impact of advanced practice providers (APPs) on their future employment.
As for physician assistants, nearly 13,000 PAs practice emergency medicine, but it is not clear if or how many are practicing independently, but, obviously, they manage patients who would be cared for by emergency physicians in the past.
How did we get here, and where are we going? Nurse practitioners and physician assistants seemed like a good idea 20 years ago when there was a drastic shortage of health care providers and a projection for more significant deficits in the coming decades. The traditional model of university-based medical school and graduate medical education was not capable of fixing this shortfall due to its Byzantine process of expansion.
But market economies thrive by exploiting a crisis, and physician medical education became a lucrative business over the past decade. More and more new private medical schools opened, and would-be doctors were eager to fork over hundreds of thousands of dollars. The subsequent increase in medical school graduates opened the door to creating more post-graduate residency training in emergency medicine. Fueled by large health care corporations with bottomless pockets, the number of EM residency programs skyrocketed.
What has evolved are two competing forms of EM health care providers. One requires considerably more training, creates a higher level of expertise, and is more expensive for the employer. The other requires less clinical training and has less expertise, but is much cheaper for the employer. What is apparent is rather than working in harmony to provide good patient care, these two factions are preparing to battle for their share of a limited pot of money.
After the Match: NPs Pushing Expansion of Independent... : Emergency Medicine News
An abstract is unavailable.journals.lww.com
Bullshi* on several accounts.
1. This isn’t about two groups of special interests fighting over a pot of money. It’s about patients being short changed by inadequately trained providers and charged for the expertise of higher level care
2. It’s also about unsafe staffing levels by the appropriate level of care, I.e. physician led care
3. The backlash on social media wasn’t “ugly” it was completely appropriate, and the residencies who were participating should be publicly shamed
4. I’m happy the next generation of students is starting to do their due diligence. It’s a really important question.
- Joined
- Mar 1, 2010
- Messages
- 24,342
- Reaction score
- 36,587
I like it more when money and people's well being form a tag team. Like when Merck decided that the most ethical way to make money was to produce their competitors vaccine 'for the good of america.'If anyone has paid attenion in the US, you'd very easily have your answer. When it comes to money vs people's well-being, money will win 110/100.
- Joined
- Jul 27, 2013
- Messages
- 38,498
- Reaction score
- 75,461
I don't really get the desire to shame places that offer these PA training programs. They're basically just OTJ training that is structured for physician assistants, I'll take that over them going out into the world with no added experienceBullshi* on several accounts.
1. This isn’t about two groups of special interests fighting over a pot of money. It’s about patients being short changed by inadequately trained providers and charged for the expertise of higher level care
2. It’s also about unsafe staffing levels by the appropriate level of care, I.e. physician led care
3. The backlash on social media wasn’t “ugly” it was completely appropriate, and the residencies who were participating should be publicly shamed
4. I’m happy the next generation of students is starting to do their due diligence. It’s a really important question.
- Joined
- Apr 22, 2006
- Messages
- 2,794
- Reaction score
- 2,625
Huh? Have you been to any large academic institution in an urban area? It may not be 90/10 split, but it’s getting close to 50/50.Rural, yes. Urban, not even close.
- Joined
- Apr 27, 2014
- Messages
- 863
- Reaction score
- 1,501
I don't really get the desire to shame places that offer these PA training programs. They're basically just OTJ training that is structured for physician assistants, I'll take that over them going out into the world with no added experience
The issue is that these places advertise themselves as training pas alongside residents in the same esi level patients and specifically sell themselves as giving high risk procedure training to pas.
There are limited numbers of these procedures, even at high volume centers (which a lot of them are not) and there is no such thing as getting “enough” of them in training. Similarly there’s no such thing as enough training in critically ill undifferentiated patients, which are common in the Ed but not so common we should give away the opportunity to learn on them.
I don’t care if pas want to train for additional time in the ed for the patients who they ultimately are appropriately trained to see and staff: esi 4,5 and occasional 3s. I do have a huge problem with blurring the lines by calling it a residency and diluting the training of your own residents to do so.
- Joined
- Sep 16, 2010
- Messages
- 1,295
- Reaction score
- 2,174
I've said this before, but it bears repeating.
The only way for this PLP problem to be resolved is to give them the rope and let them tie their own noose.
Refuse to train them, refuse to supervise them, don't work for hospitals that do.
Let the attorneys feast on their incompetence, and let the public outcry be "we want to see the doctor".
Yeah, its going to be painful for us; but it will be worth it in the end.
We need to diversify ourselves in Birdstrike like fashion until then.
EDIT: Oh, and ACEP needs to be erased. Altogether.
Agree with you 1000%. The forces capable of reigning in the PA/NP mayhem are law and money.
Law: Pretty self explanatory as you allude to. Enough patients are harmed that laws are made to protect the public.
Money: Things evolve in such a way that it becomes widely appreciated by the public and lawmakers that PA/NPs often don't offer "a cost savings" when you factor in all the superfluous testing/treatment/medical misadventures/referrals/inefficiencies they generate + the growing costs of their medmal liability. The key is that you'd need to figure out a way to have the individual hospital/employer +/- patients pay the financial burden of these excess costs, rather than the current model where the larger health care "system"/abyss just sort of absorbs it.
- Joined
- May 29, 2015
- Messages
- 2,402
- Reaction score
- 6,276
I don't really get the desire to shame places that offer these PA training programs. They're basically just OTJ training that is structured for physician assistants, I'll take that over them going out into the world with no added experience
Because for what? They can handle strep and bronchitis after PA school. There's 100% no reason they need to see hard level 3s or do any kind of resuscitation. That's what we're for.
- Joined
- Sep 27, 2008
- Messages
- 3,015
- Reaction score
- 2,223
I'm honestly not convinced this is true. Witness all the unnecessary strep screens for every fever/cough/belly pain leading to over-diagnosis and treatment of carriers or rampant levofloxacin for anyone w/ a cough.Because for what? They can handle strep and bronchitis after PA school. There's 100% no reason they need to see hard level 3s or do any kind of resuscitation. That's what we're for.
I mean, personally I wasn't prepared to work in fast track unsupervised during my intern year, so why would I expect midlevels to be?
- Joined
- Jul 27, 2013
- Messages
- 38,498
- Reaction score
- 75,461
Because for what? They can handle strep and bronchitis after PA school. There's 100% no reason they need to see hard level 3s or do any kind of resuscitation. That's what we're for.
Yeah, pretty much what I was going to say. The thing about PAs is they used to be carefully selected former clinicians with very rigorously structured programs that went into limited roles under high levels of supervision. They aren't cut out for doing much of anything straight out without someone working to train them, and that training being structured is preferable to notI'm honestly not convinced this is true. Witness all the unnecessary strep screens for every fever/cough/belly pain leading to over-diagnosis and treatment of carriers or rampant levofloxacin for anyone w/ a cough.
I mean, personally I wasn't prepared to work in fast track unsupervised during my intern year, so why would I expect midlevels to be?
- Joined
- May 29, 2015
- Messages
- 2,402
- Reaction score
- 6,276
I'm honestly not convinced this is true. Witness all the unnecessary strep screens for every fever/cough/belly pain leading to over-diagnosis and treatment of carriers or rampant levofloxacin for anyone w/ a cough.
I mean, personally I wasn't prepared to work in fast track unsupervised during my intern year, so why would I expect midlevels to be?
Yeah, pretty much what I was going to say. The thing about PAs is they used to be carefully selected former clinicians with very rigorously structured programs that went into limited roles under high levels of supervision. They aren't cut out for doing much of anything straight out without someone working to train them, and that training being structured is preferable to not
Right, because of their year of fake "residency" they'll say they're now qualified for fast track. Please. They'll use that useless time to justify to clueless admins and CMGs they can independently run resus/2s/3s, etc
- Joined
- Dec 19, 2010
- Messages
- 10,255
- Reaction score
- 13,584
Merck is doing what’s best for Merck.I like it more when money and people's well being form a tag team. Like when Merck decided that the most ethical way to make money was to produce their competitors vaccine 'for the good of america.'
Merck’s vaccines failed. They didn’t work and therefore Merck can’t make money off Merck’s COVID vaccine, so they abandoned it. Merck, being run by smart businessmen, found a way to get paid (by the US taxpayers) to produce a vaccine developed by another company. Smart.
I’m glad Merck is producing someone else’s vaccine. Still, I won’t let that mislead me into believing Merck is doing it for “ethics.” Merck is in business to make money, not to be ethicists.
Last edited:
- Joined
- Jul 6, 2008
- Messages
- 3,477
- Reaction score
- 5,974
There is nothing a company does that does not involve the end result of making money. No company cares much about ethics nor should they. They are built to make money, maximize profits, and return investor equity.
If "doing something for free" or "doing something for the good" comes with good free press, then they will sacrifice profits knowing they will make more from good will. But never would they do something for free unless they are getting something back eventually.
If "doing something for free" or "doing something for the good" comes with good free press, then they will sacrifice profits knowing they will make more from good will. But never would they do something for free unless they are getting something back eventually.
- Joined
- May 2, 2010
- Messages
- 764
- Reaction score
- 596
BoomersWow imagine voting in a mid-level, just to watch them literally turn around and lay you off. How stupid can you be.
- Joined
- Nov 21, 2003
- Messages
- 3,355
- Reaction score
- 2,833
The expansion of MLPs are a classic example of what happens when the benefits of a decision go to one group, and the costs fall on other groups. MLPs are cheap for the CMG/hospital in terms of initial salary, certainly they're more than 15% cheaper than docs which is the difference in billing for a lot of insurances. But they're expensive in terms of testing, they're expensive in terms of consultant utilization. In systems where those expenses are felt by the hospital, there are very few MLPs. In systems where those expenses are externalized, they thrive.
But they're expensive in terms of testing, they're expensive in terms of consultant utilization. In systems where those expenses are felt by the hospital, there are very few MLPs. In systems where those expenses are externalized, they thrive.
You are conflating general costs to costs borne by the hospital. More imaging and more consulting is a perk not a drawback to midlevels because of our mostly fee for service model. The ER doc who correctly triages, diagnoses, and discharges a patient without advanced imaging or consults makes the hospital system less money than the midlevel who consults and CTs everyone. In the grand scheme, it adds stress and cost to the health system, but to the hospital system, they couldn't care less. They are profiting massively off midlevels.
Things that can change this calculus are moving towards an outcomes/best practices/capitation model. Then the utility of an MD becomes apparent as inappropriate imaging is less likely to occur, inappropriate consults are less likely to occur, and the patients are dispo'ed correctly, netting the system cost savings and the hospital more profits.
- Joined
- Nov 21, 2003
- Messages
- 3,355
- Reaction score
- 2,833
Read my post again. Then consider if your initial statement is accurate.You are conflating general costs to costs borne by the hospital. More imaging and more consulting is a perk not a drawback to midlevels because of our mostly fee for service model. The ER doc who correctly triages, diagnoses, and discharges a patient without advanced imaging or consults makes the hospital system less money than the midlevel who consults and CTs everyone. In the grand scheme, it adds stress and cost to the health system, but to the hospital system, they couldn't care less. They are profiting massively off midlevels.
Things that can change this calculus are moving towards an outcomes/best practices/capitation model. Then the utility of an MD becomes apparent as inappropriate imaging is less likely to occur, inappropriate consults are less likely to occur, and the patients are dispo'ed correctly, netting the system cost savings and the hospital more profits.
- Joined
- Sep 19, 2004
- Messages
- 2,950
- Reaction score
- 3,279
Does kaiser lose money on testing?The expansion of MLPs are a classic example of what happens when the benefits of a decision go to one group, and the costs fall on other groups. MLPs are cheap for the CMG/hospital in terms of initial salary, certainly they're more than 15% cheaper than docs which is the difference in billing for a lot of insurances. But they're expensive in terms of testing, they're expensive in terms of consultant utilization. In systems where those expenses are felt by the hospital, there are very few MLPs. In systems where those expenses are externalized, they thrive.
- Joined
- Nov 21, 2003
- Messages
- 3,355
- Reaction score
- 2,833
In a fully capitated system, you lose money on any care you provide. So whether you save or spend money on a specific test would depend on whether that test is less expensive than the downstream consequences. A $1000 CTCA that prevents a $2000 cardiac cath 3/4's of the time would be a money saver, A respiratory pathogen panel that costs $950 and prevents an unnecessary $10 amox script 3/4's of the time would be a money loser. It can get tough when you start trying to add 2nd and 3rd order effects (repeat visits, hospitalization rates, costs of rare complications, and in non EPO/HMO settings leakage rate). In a capitated system, the most dangerous thing you can do monetarily is have a provider that has access to a broad range of tests and is being incentivized by outside sources (ie. medmal/patient satisfaction) to use them.Does kaiser lose money on testing?
D
deleted941485
In a fully capitated system, you lose money on any care you provide. So whether you save or spend money on a specific test would depend on whether that test is less expensive than the downstream consequences. A $1000 CTCA that prevents a $2000 cardiac cath 3/4's of the time would be a money saver, A respiratory pathogen panel that costs $950 and prevents an unnecessary $10 amox script 3/4's of the time would be a money loser. It can get tough when you start trying to add 2nd and 3rd order effects (repeat visits, hospitalization rates, costs of rare complications, and in non EPO/HMO settings leakage rate). In a capitated system, the most dangerous thing you can do monetarily is have a provider that has access to a broad range of tests and is being incentivized by outside sources (ie. medmal/patient satisfaction) to use them.
You make algorithms that MLPs can follow and give them a very narrow choice of options. Done.
- Joined
- Feb 4, 2017
- Messages
- 888
- Reaction score
- 1,343
Yes I believe Kaiser straight up shut down an ER doc for giving doxy, ivermectin etc to covid patients. The providers are meticulously tracked it seems.You make algorithms that MLPs can follow and give them a very narrow choice of options. Done.
D
deleted941485
Yes I believe Kaiser straight up shut down an ER doc for giving doxy, ivermectin etc to covid patients. The providers are meticulously tracked it seems.
Its bascially how you can get around having MLPs go wild with the testing. Just severely limit their choices. Instead of going thrugh an insurance company for approval your Mega Health Systems IT department will cut you off at the level of orders.
- Joined
- Apr 22, 2006
- Messages
- 2,794
- Reaction score
- 2,625
Its bascially how you can get around having MLPs go wild with the testing. Just severely limit their choices. Instead of going thrugh an insurance company for approval your Mega Health Systems IT department will cut you off at the level of orders.
If they do that then they'll have to crunch the numbers to see if malpractice payout/insurance premiums would cover the difference between midlevel and physician. Many MLPs (and physicians) use ordering of tests to make up for clinical deficiencies. If you take that away, then you're essentially taking off the training wheel, and allowing full consequence of said deficiencies - one of which is malpractice cost paid by employer.
D
deleted941485
If they do that then they'll have to crunch the numbers to see if malpractice payout/insurance premiums would cover the difference between midlevel and physician. Many MLPs (and physicians) use ordering of tests to make up for clinical deficiencies. If you take that away, then you're essentially taking off the training wheel, and allowing full consequence of said deficiencies - one of which is malpractice cost paid by employer.
With all the money they can skim. If the avg out of court settlement is reasonable cost of doing business for few dead patients then so be it. have 1 doc overseeing the entire ER and a slew of MLPs. This is an admin's wet dream. Plus many states have already removed the training wheels.
They have alot of the pieces already.
- Joined
- Aug 17, 2002
- Messages
- 2,501
- Reaction score
- 1,130
If they do that then they'll have to crunch the numbers to see if malpractice payout/insurance premiums would cover the difference between midlevel and physician. Many MLPs (and physicians) use ordering of tests to make up for clinical deficiencies. If you take that away, then you're essentially taking off the training wheel, and allowing full consequence of said deficiencies - one of which is malpractice cost paid by employer.
If I recall correctly, the main reason we didn't use mid-levels in the ED at KPNW was more related to their ability to join and have union representation – a greater challenge to having the typical bulletproof staffing required.
It's fair to say there's a value to a clinician in resource stewardship versus a lesser-trained mid-level, but, really, all it takes are well-defined clinical pathways with a doc available for consultation on complex cases and you'll be set for 99% of medicine.
I'm a first year student and have been trying to understand the saturation/employment problem in EM. How does primary care docs being employed in the ED impact this? Prior to matriculating I was a paramedic in the Florida panhandle. Most of the hospitals in the area are considered rural. Almost all of the docs in the ED were primary care, either IM or FM. Are they there because of a localized shortage of EM trained docs?
- Joined
- May 29, 2015
- Messages
- 2,402
- Reaction score
- 6,276
I'm a first year student and have been trying to understand the saturation/employment problem in EM. How does primary care docs being employed in the ED impact this? Prior to matriculating I was a paramedic in the Florida panhandle. Most of the hospitals in the area are considered rural. Almost all of the docs in the ED were primary care, either IM or FM. Are they there because of a localized shortage of EM trained docs?
Because EM was created in the 1980s. So it's relatively new. Before then, random physicians and residents staffed the ED. FM, IM, surgery. As em became a specialty, we started properly taking over starting at larger centers, etc. Historically, rural EDs were not staffed by boarded EM docs initially because of supply back in the day. Then somewhat more recently was because they just couldn't pay the going rate. Now boarded/eligible EM docs have nowhere else to go so they're filling these rural places.
NonEM docs typically are currently limited to rural places unless they've been grandfathered into a more busy place. Overtime nonEM docs will go away quickly from EDs as our oversupply continues. My large hospital system that owns many small hospitals for the past several years has been phasing out and in some cases straight firing nonABEM docs from EDs and they're already full of BCEM docs.
Did we need more EM docs? Probably 10 years ago, but not anymore. Have to have an adequate balance of supply and demand but that's been overshot by several hundred positions per year excess at minimum, mainly thanks to CMGs. I expect within the next 4-5 cycles, we'll have fully unemployed new grads.
- Joined
- Feb 4, 2017
- Messages
- 888
- Reaction score
- 1,343
Yes plus I believe if you join Kaiser you have to agree to arbitration for med mal.With all the money they can skim. If the avg out of court settlement is reasonable cost of doing business for few dead patients then so be it. have 1 doc overseeing the entire ER and a slew of MLPs. This is an admin's wet dream. Plus many states have already removed the training wheels.
They have alot of the pieces already.
- Joined
- Feb 22, 2014
- Messages
- 281
- Reaction score
- 189
4-5 cycles? I’m worried it’s closer to 1-2.Because EM was created in the 1980s. So it's relatively new. Before then, random physicians and residents staffed the ED. FM, IM, surgery. As em became a specialty, we started properly taking over starting at larger centers, etc. Historically, rural EDs were not staffed by boarded EM docs initially because of supply back in the day. Then somewhat more recently was because they just couldn't pay the going rate. Now boarded/eligible EM docs have nowhere else to go so they're filling these rural places.
NonEM docs typically are currently limited to rural places unless they've been grandfathered into a more busy place. Overtime nonEM docs will go away quickly from EDs as our oversupply continues. My large hospital system that owns many small hospitals for the past several years has been phasing out and in some cases straight firing nonABEM docs from EDs and they're already full of BCEM docs.
Did we need more EM docs? Probably 10 years ago, but not anymore. Have to have an adequate balance of supply and demand but that's been overshot by several hundred positions per year excess at minimum, mainly thanks to CMGs. I expect within the next 4-5 cycles, we'll have fully unemployed new grads.
Anyone else know any current PGY-3s who still can’t find jobs?
- Joined
- Nov 12, 2009
- Messages
- 4,830
- Reaction score
- 2,702
A number at my old program have only been able to obtain part time employment -- about 3 months from graduating. I dont know what the details of those positions consist of...
Better than unemployed I suppose. At least they can service their loans. Sad to see.
Better than unemployed I suppose. At least they can service their loans. Sad to see.
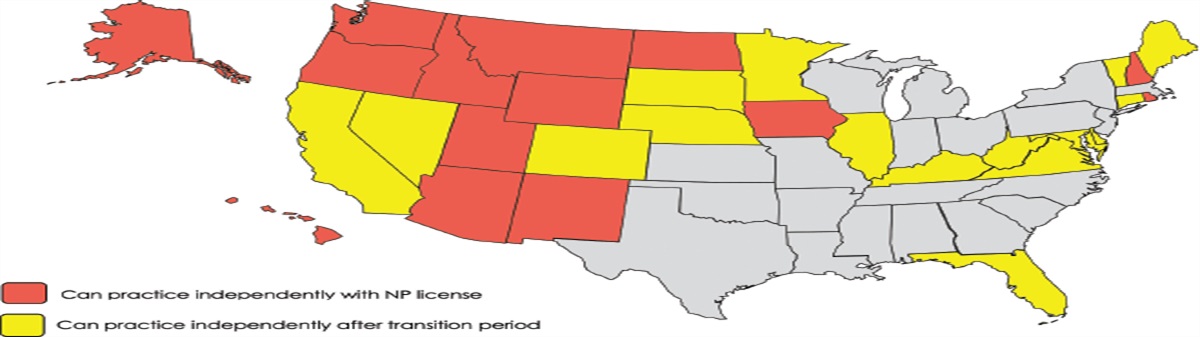
Even in states with np's practicing independently hospitals still like having physicians supervise to carry the liability for anything that goes wrong.With all the money they can skim. If the avg out of court settlement is reasonable cost of doing business for few dead patients then so be it. have 1 doc overseeing the entire ER and a slew of MLPs. This is an admin's wet dream. Plus many states have already removed the training wheels.
They have alot of the pieces already.

