- Joined
- Nov 21, 1998
- Messages
- 12,707
- Reaction score
- 7,157
If I were a placebo KOL, believed in the power of intentional healing, or psychokinetic properties of local anesthetics, I'd be pissed...
"The strength of this trial is that nearly all participants (94%) were convinced they received the actual cementation, with no crossovers. In other words, the placebo effect (expectations of pain relief) was high, but nevertheless, PV was significantly better than active control (placebo) for pain and health-related quality of life."
"Compared with active control, percutaneous vertebroplasty (PV) intervention led to pain reduction and better health-related quality of life in participants with chronic osteoporotic vertebral compression fracture. We believe that future research should focus on PV versus true sham intervention in a multicenter trial with at least 1 year of follow-up."
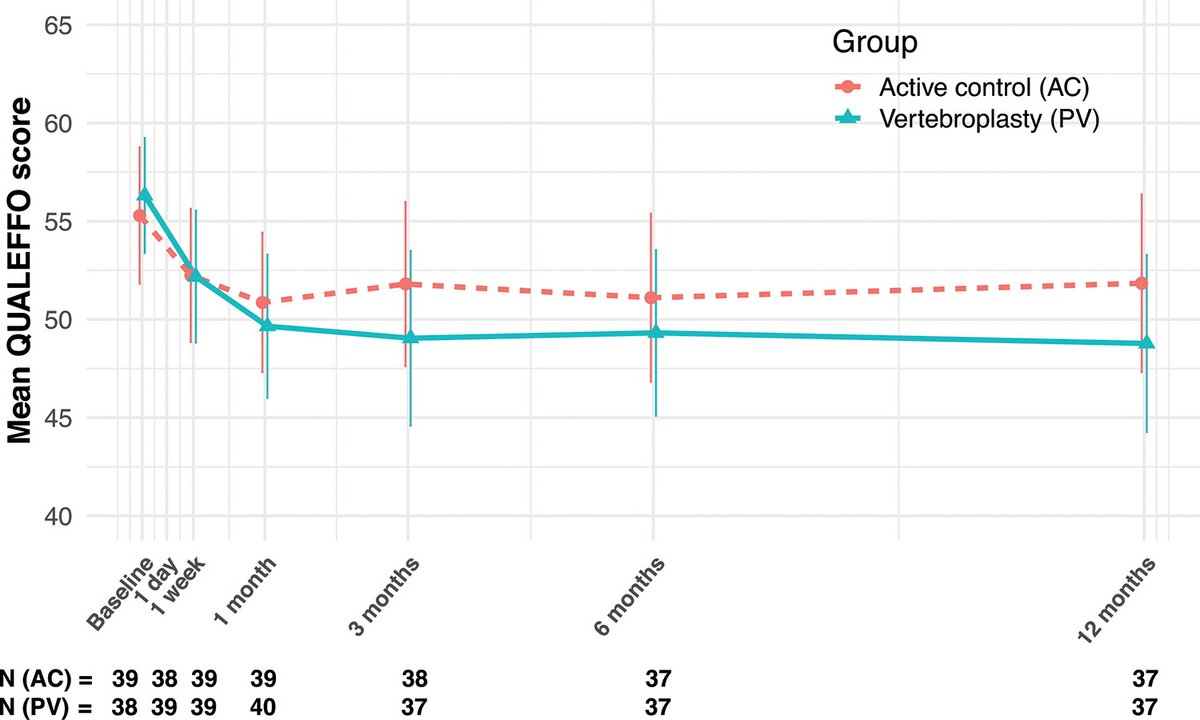
"The strength of this trial is that nearly all participants (94%) were convinced they received the actual cementation, with no crossovers. In other words, the placebo effect (expectations of pain relief) was high, but nevertheless, PV was significantly better than active control (placebo) for pain and health-related quality of life."
"Compared with active control, percutaneous vertebroplasty (PV) intervention led to pain reduction and better health-related quality of life in participants with chronic osteoporotic vertebral compression fracture. We believe that future research should focus on PV versus true sham intervention in a multicenter trial with at least 1 year of follow-up."
Last edited:
