What are your thoughts on anti-IL6 and anticoagulants?
I'm not on the cutting edge of the research on these two topics, but I'll answer to the best of my ability.
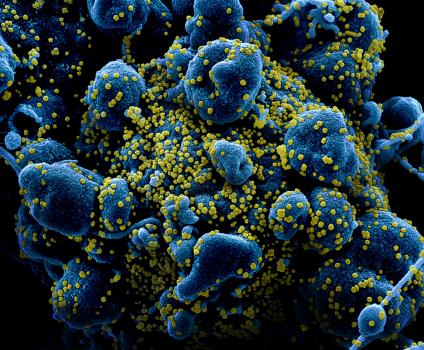
Considering COVID-19 seems to have a
pro-coagulant effect, it doesn't surprise me that anti-coagulation is showing promise in these patients. More study is needed, obviously, to determine if the effect is real, for which patients, when, what drug and what dose. The one paper in the
Journal of American Cardiology did show a big enough mortality difference difference it can't be ignored (29% mortality, vented patients on anti-coagulation vs 62% mortality of vented patients not on anti-coagulation).
Interestingly, guess what else has an anti-coagulant effect? Hydroxychloroquine, through
platelet inhibition. That's one of it's benefits in Lupus. So if it has a positive effect in COVID-19, it may be by this mechanism alone. Either way, it seems to me the use of anti-coagulants has to be looked at.
As far as IL-6, it's also an interesting approach. Like most everything with COVID-19 being so new, what do we have? A mix of small, non-controlled trials which yet don't prove anything one way or the other, yet, right? But I did read about a small study out of France with one of the IL-6 blockers which was positive and then a different one, with a different drug by a different maker, which showed negative results.
So, I don't know. It's all new, evolving and changing every day, isn't it? The only thing I know for sure about COVID-19, is that there's a lot to learn about COVID-19, by just about everybody, myself included.




 )
)