Yeah, I think we're going to pretty significantly disagree on the whole "shared decision making isn't something I value with my patients" thing... So you did discuss APBI, but didn't document it as an option? I will correct a resident who 1) documents something that was not done or 2) does not document something that was done and is clinically relevant.
Observation not an option for this low-risk DCIS patient as per RTOG 9804? Because of a LC benefit?
Do all of your 65-70+ T1N0 IDC patients get RT too, no discussion about observation?
How does anyone know you talked about side effects? The amount of times I've seen a patient in follow-up or covering and the patient has ZERO idea of what toxicities to expect is astronomically high. The PCPs are not calling you about RT toxicity because they're telling their patients it's because of it! This is like the entire reason we still have so many people in the current generation who as either laymen or even other physicians are so incredibly biased against RT.
If you write a barebones note in a paternalistic manner with zero description of the thought process and lack of nuance necessary for clinical situations, it makes you sound like a boomer rad onc. Now you and I both know that you're not a boomer rad onc when it comes to planning based on your post history, but how would you expect anyone who reads THAT A/P to think that you would do anything differently than a boomer?
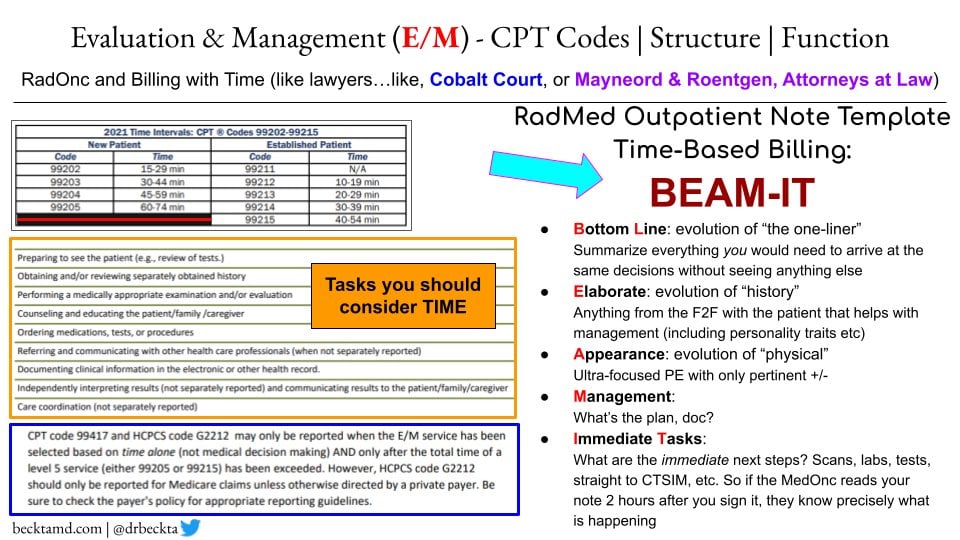
Your note sounds like this to me: "Patient has L Breast DCIS. Got surgery. To receive radiation. Thank you for this interesting consult." Bill 99205.
That's an opinion. Not one I agree with

You can just call people Boomer that do things you disagree with, but true Boomers are the ones writing these long notes. This is like when people started saying "literally" when they meant it not literally.
I see a long note with all that stuff in it, and I see inefficiency, note bloat and inefficient communication. It really frustrates me. I'm board certified. I don't need to read about 9804 in your note. I see a lot of that from young docs, showing how recently they took their exams. It is ... something.
Observation is an option. RT is category 1. I was consulted for my opinion. I gave it

For stage I, I've tweeted about this and talked about it - if you can get a screening mammo, diag mammo, biopsy, lump +/- SLN, even think about ET for 5 years, you can get RT for 5 days. It is category 1. I bring up observation and then I say, "in my opinion the reduction of IBTR is worth it".
I said I talked about side effects. They are well documented.
It's interesting about PCPs - I'm setting up shop in one, 1/2 a day every other week starting this month. We have excellent relationships with them. If you talk to them, spend time in their office, they really get to learn about what we do. Most don't have time to read the long notes where the toxicity is listed in a paragraph 5 pages deep.
I like your last sentence. That is a good note! I would understand completely.
Sean McBride says his consult is tweet length. I don't think he's a Boomer.
Also: nuance for breast cancer? Have you not seen my algorithm?