Hi
M1 here.
We recently had a chance to diagnose standardized patients. This was the first time they had let us workup a patient and turn it into a diagnosis. I found it really exciting and realized that this is why I wanted to do medical school.
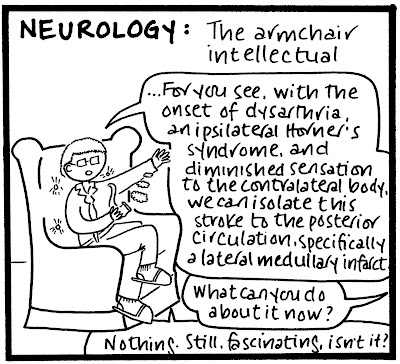
What are the best specialties or fields for doing this kind of work. Just simply meeting patients, hearing their stories, putting the clues together and diagnosing.
Is this family medicine or internal? General medicine or some specialty or maybe even path?
I'm really attracted to the Sherlock Holmes concept of a physician; detective work, clinical reasoning etc. I recently found out about Faith Fitzgerald and was super inspired by her lectures.
Thanks SDN
M1 here.
We recently had a chance to diagnose standardized patients. This was the first time they had let us workup a patient and turn it into a diagnosis. I found it really exciting and realized that this is why I wanted to do medical school.
What are the best specialties or fields for doing this kind of work. Just simply meeting patients, hearing their stories, putting the clues together and diagnosing.
Is this family medicine or internal? General medicine or some specialty or maybe even path?
I'm really attracted to the Sherlock Holmes concept of a physician; detective work, clinical reasoning etc. I recently found out about Faith Fitzgerald and was super inspired by her lectures.
Thanks SDN
Last edited: