- Joined
- May 30, 2006
- Messages
- 203
- Reaction score
- 124
First time I have reason to do a true extrapedicular kypho. 60 y/o M on chronic glucocorticoids presents with severe low back pain. Edema noted at L3 and L4, patient with prior instrumented fusion at L4-5.

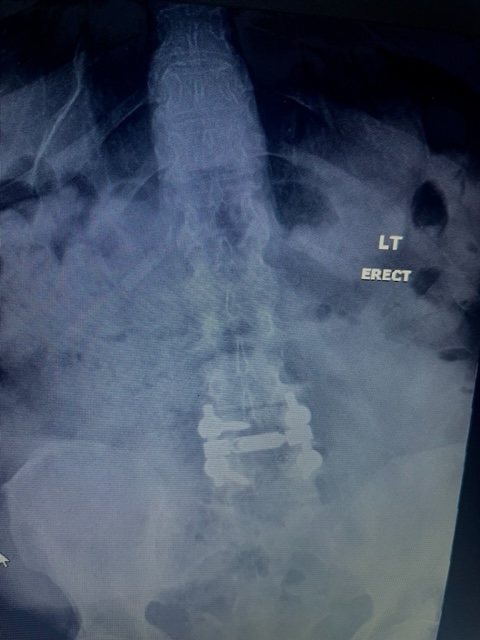

Screws are fairly superior at L4, so I was planning on using Beall's extrapedicular inferior end plate access, aka low and outside (3rd picture).
Since I hadn't augmented a fused level before, Stryker connected me to one of their KOLs. He was obviously an IR guy who did many of these under CT. He actually recommended that after augmenting L3, using the curved needle to go through the L3-4 disc and injecting cement into L4 that way. He also mentioned that if he gets into bleeding going extrapedicular, he will place in some Gelfoam or Surgicel. All this made me kind of nervous. I am but a simple country pain doc who does in-office kyphos under local and oral meds. Beall makes extrapedicular access sound easy, but I'm not trying to be a cowboy if this is some big ordeal. Any experience docs with thoughts or suggestions?
Screws are fairly superior at L4, so I was planning on using Beall's extrapedicular inferior end plate access, aka low and outside (3rd picture).
Since I hadn't augmented a fused level before, Stryker connected me to one of their KOLs. He was obviously an IR guy who did many of these under CT. He actually recommended that after augmenting L3, using the curved needle to go through the L3-4 disc and injecting cement into L4 that way. He also mentioned that if he gets into bleeding going extrapedicular, he will place in some Gelfoam or Surgicel. All this made me kind of nervous. I am but a simple country pain doc who does in-office kyphos under local and oral meds. Beall makes extrapedicular access sound easy, but I'm not trying to be a cowboy if this is some big ordeal. Any experience docs with thoughts or suggestions?