I’m not sure where you got that abstract but if it’s from SYNTAX then it’s old and not performed with the current generation of PCI platforms.. Even FAME 3 didn’t really answer the question because the freedom from MACE at one year was pretty damn close in my opinion for both CABG and PCI, and in that trial did NOT use IVUS guided PCI which improves outcomes. The CABG group in FAME3 also bled a lot more (obviously) and ended up with more post op dysrrhythmias and rehospitalization and stroke . Not to mention mandatory recovery from open heart surgery which is unavoidable.
Also although I hate to bring this up, You have to also consider how politicized science and medicine is. The best you can say is that the data, if you take it at face value, “supports” CABG when the vessels are awful candidates for PCI (this will not last forever). And the resistance to other conclusions may have political motivations .
The fact of the matter is CABG involves cracking chests and risking stroke, new dysrrhythmic disorders, and pain and suffering far in excess of PCI, for not-yet truly proven superiority in CAD. I exercise every day, and I cannot continue to be an anesthesiologist if I have a massive stroke. If I develop an Impossible to ablate atrial arrhythmia as a result of my atriotomy I will be really unhappy. Given my choices today, I personally would have a PCI in almost all circumstances.
@sevoflurane posts regarding the nebulous longer-term outcomes of TAVR are almost identical to the issues that plague PCI.
I've been hearing about how the next generation stent will be the latest and greatest thing for the last 15 years, and yet while the outcomes in the short-term in complex patients are equivocal (due to the periop risks of CABG), CABG is
significantly better at 5, 10, 15, 20 years, etc. Because of the aforementioned advantages of using living arterial tissue as a graft.
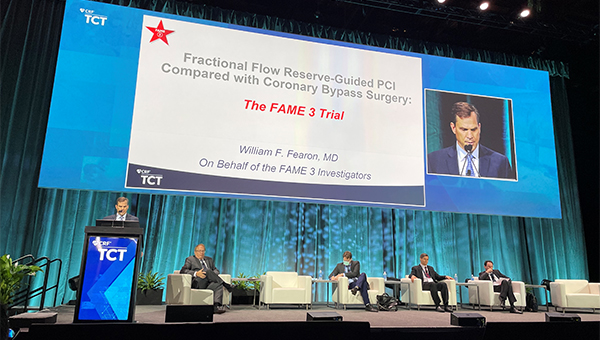
Wrt FAME 3, literally every investigator was dead certain that PCI was going to be non-inferior to CABG when they were designing the trial, and yet:
Overall results found the primary endpoint of death, MI, stroke or repeat revascularization was 10.6% in the PCI group compared with 6.9% in the CABG group at one year. In addition, the incidence of death, MI, or stroke was 7.3% in the FFR-guided PCI group compared with 5.2% in the CABG group.

www.acc.org
Marc Ruel, MD (University of Ottawa Heart Institute, Canada), said the results of the trial took him by surprise.
“Personally, I was wrong,” he told TCTMD. “I really thought that the 1-year results of FAME 3 would show noninferiority. I’d been saying this to many people because when you look at SYNTAX, FREEDOM, NOBLE, and EXCEL—the four main trials [comparing CABG versus PCI]—the event curves start separating at 2 to 3 years. In SYNTAX, there was no difference at 1 year. In EXCEL, there was no difference, same with NOBLE. In FREEDOM, it took 2 or 3 years for the curves to separate.”
Given the early separation of the event curves in FAME 3, Ruel, like Kirtane, expects the difference in clinical outcomes will be even more pronounced in long-term follow-up.
In terms of why FAME 3 failed to show PCI was noninferior to surgery, Ruel said surgeons are getting better at performing the procedure, with an increased focus on reducing the risk of adverse events, particularly the risk of stroke. The surgical techniques used by operators in FREEDOM and SYNTAX are now outdated, he added, noting that since those trials were published the surgical community has initiated sweeping quality-improvement initiatives.
(UPDATED) Interventionalists and surgeons call it a big win for CABG surgery, especially since its advantages were seen so early.

www.tctmd.com
And maybe IVUS helps, maybe it doesn't. There are not a bunch of large, randomized trials establishing that. Hence why it's a class II recommendation. Same as FFR, except FFR/iFR probably has an order of magnitude more trials establishing its utility.
Where we agree is that CABG needs to evolve. We don't do open cholecystectomies any more, so given technological advancement it's just not reasonable to expect that CTS is absolved of having to learn complex endoscopic and robotic techniques. I'm almost 40 years old. I have a very strong family history of CAD. Like you, I do not want a sternotomy, but I think that's it's essentially inarguable that anything is going to confer a longer long-term survival advantage than a LIMA-LAD.
I think by the time I need a CABG, if GDMT has not cured CAD or the propensity for plaques to rupture, I suspect I will be getting a hybrid procedure (TECAB or MIDCAB for the LIMA-LAD + PCI to the other lesions)