I work in the community and in my last job we had some extremely well trained NPs running the ICU at night and doing the majority of the work during the day for the Pulm group. In fact, two of them are being sent over to a new hospital to run the ICU with minimal attending involvement. I trained two of them in the ED before they went upstairs and joined the ICU. I wish I could say terrible things about them but they really know their stuff and I'd let them take care of me before I'd let some of my old colleagues. I got called up twice for airway disasters and both were legit. One turned into a cric in a rotoprone bed and another one was a guy who had so much vocal cord edema that I could barely get the bougie through and had to muscle a 6.0 tube so hard I thought I was going to dissect his trachea.
We all like to assume that NP/PAs can't learn to do this stuff as well as we can. As if our training or innate skill, talent, smarts, whatever...precludes them from mastering our skillset and that's where you are flat wrong. It's GREED and LAZINESS that will ultimately destroy us. Training them to staff the ICU/ED at night, work the odd/less desirable hours, ease the workload, cut a doc here, cut a doc there, pay the NP/PA less so that the senior partners can make more money. Destroying and eroding our future in the process. The irony is that we watched anesthesia drive themselves off a cliff and here we are doing the exact same thing. If we lose our salaries and specialties to MLPs, we have only ourselves to blame.
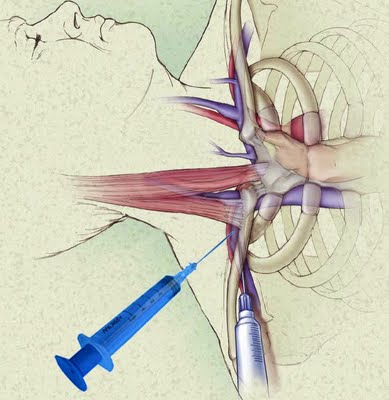
I had an ICU PA last shift asking me to teach him how to do a subclavian line because NSGY fellow had requested one for their SAH pt with an EVD because he didn't want venous outflow obstruction from an IJ CVL. (WTF?) I kindly turned him down on a bedside teaching opportunity and stated I would take care of it for him. When he left, I popped one in by myself. I closely guard my skillset and as much as I respect and genuinely enjoy working with MLPs, hey...this is business and I'd like to keep my job thank you very much!