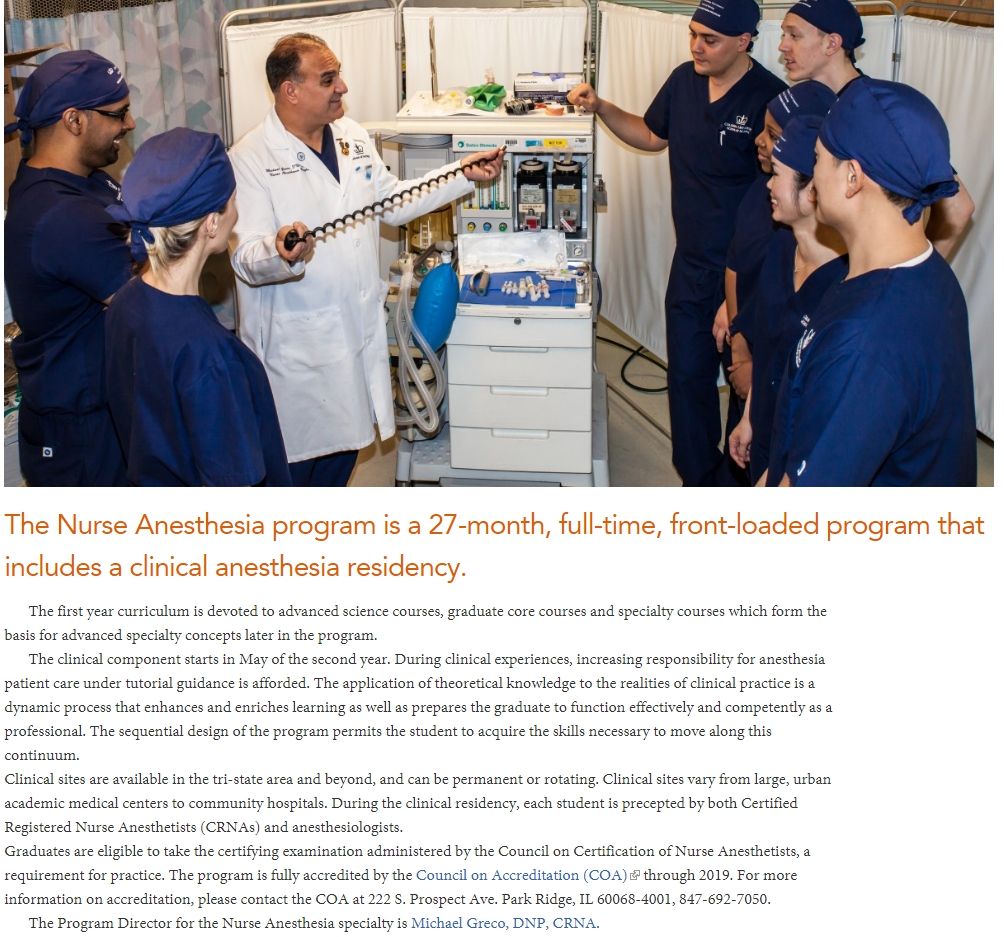
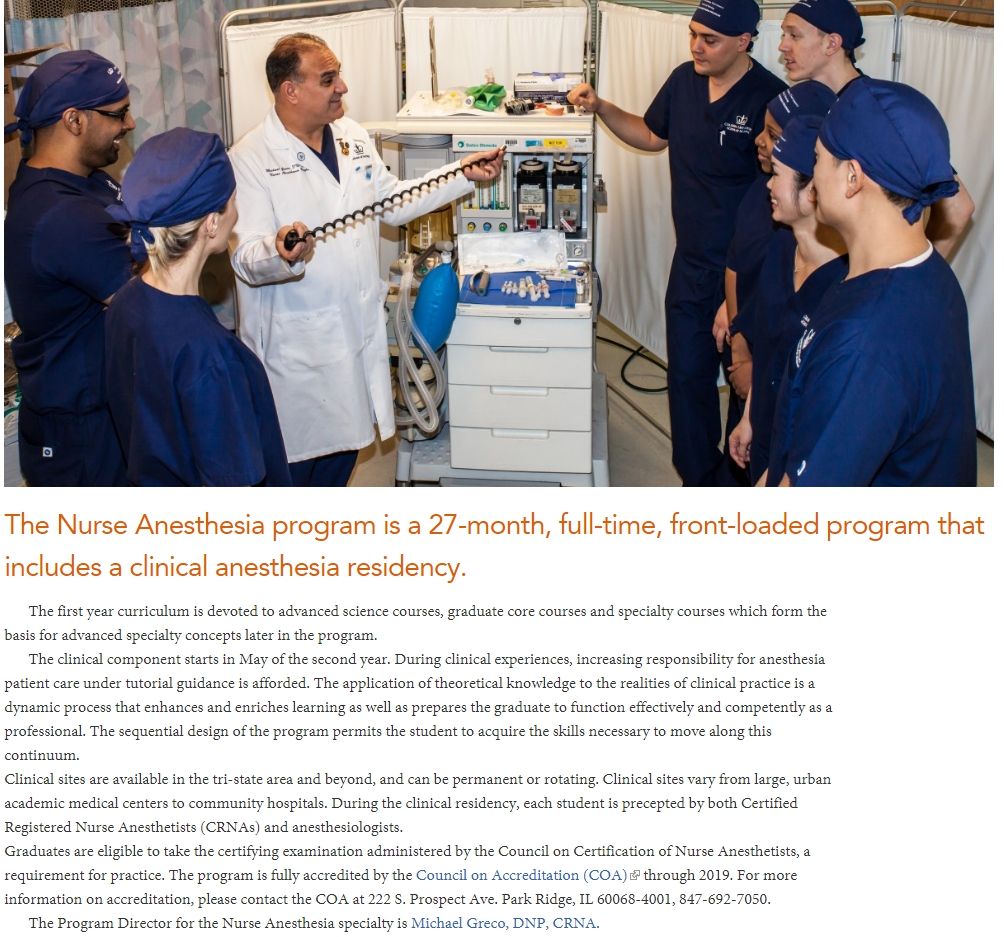
Don't these clowns realize they're in direct violation of AORN standards if they wear this attire into the OR? Shocking. 😉It looks like it's already kind of starting to happen! For example, see this article from Columbia University's School of Nursing.
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
SRNAs introducing themselves as residents
- Thread starter j bones
- Start date
Don't these clowns realize they're in direct violation of AORN standards if they wear this attire into the OR? Shocking. 😉
Jwk my favorite AA. We will try again this year to get AAs approved in my state. The dark force is strong and crafty and defeated us in committee for the bill.
We should get a bill that lays out health care naming.
- Joined
- Jan 2, 2014
- Messages
- 11,384
- Reaction score
- 24,028
- Points
- 7,061
- Location
- ヽ(´ー`)ノ
- Resident [Any Field]
It looks like it's already kind of starting to happen! For example, see this article from Columbia University's School of Nursing.
dude has a lot of flare
- Joined
- Nov 30, 2009
- Messages
- 2,011
- Reaction score
- 2,220
- Points
- 5,516
- Location
- OH
- Attending Physician
Don't these clowns realize they're in direct violation of AORN standards if they wear this attire into the OR? Shocking. 😉
That's not gonna work. Machine has to be off if they want to use that.
D
deleted59964
That is so f&$@ed upI did a pre op on a 1d old kiddo today. Guess who put the Cvl, art line, lines, intubation, chest tube than wrote the h&p.... The aprn, but the attending co signed the h&p bec they can't admit...... Yet.
We have a nicu/picu fellowship, yet the aprn did this all. Utterly disillusioned with medicine at this point in training.
D
deleted171991
Those are all monkey skills. Even the H&P on a 1 day-old. Nobody needs a doctor for a relatively simple procedure anymore. It's not like the APRN did surgery on the patient. One could probably train a tech to insert lines.
The doctor part comes in at diagnosing and managing that patient. That's the future of critical care (not just pediatric), by the way.
The doctor part comes in at diagnosing and managing that patient. That's the future of critical care (not just pediatric), by the way.
Last edited by a moderator:
Those are all monkey skills. Even the H&P on a 1 day-old. Nobody needs a doctor for a relatively simple procedure anymore. It's not like the APRN did surgery on the patient. One could probably train a tech to insert lines.
The doctor part comes in at diagnosing and managing that patient. That's the future of critical care (not just pediatric), by the way.
The problem is, they start thinking theyre independent clinicians because theyre doing procedures typically reserved for doctors only ie look how crna have spun that.
The icu aprn are crna militant.
- Joined
- Mar 27, 2011
- Messages
- 2,074
- Reaction score
- 2,824
- Points
- 5,636
- Attending Physician
You're right. I was a resident and I complained, but I was powerless. I hated my program because I felt that SRNA in some ways had better access to specialty cases and training sites off-limits to residents. As a CA-1 I was always doing general & urology cases, and my SRNA peers would already be doing OB, regional blocks, etc., since they have a shorter clinical training duration. I came out of residency not comfortable with simple things like epidural and blocks. So tons of classmates spent another year in fellowship, OB, regional, ... looking back, CA-1 was a complete waste of time.
I think chairmen have substantial power in steering the direction of the residency. However, at that level, they're just corrupt politicians more interested in generating revenue, promoting research and publication, enhancing the institute's ranking and reputation (often based on research volume), than truly interested in investing in the future of the profession and job competitiveness of individual graduates going into PP.
But you can start from yourself. You can work together, but you don't have to teach them. I gently tell SRNAs they're not very welcomed in my room. If they come, I don't teach much and I don't say much. I cringe when I see attending who like to show off their knowledge base and teach SRNA "residents" how to put in central lines or how to interpret TEE, as if their personal ego depends on it. This profession is a plate of scattered sand, but I do my part. I'm the power of one.
I know you've graduated by now, but residents really need to know that this is what the ACGME is for. There is a lot of bureaucracy and crap tied into the ACGME, but their true purpose is to ensure that training programs and producing competent physicians and the priority goes to residents within the training environment.
Fill out the survey properly and don't take any BS from your administration about losing credentialing. Most anesthesia residencies need their residents just as much as their residents need them (outside of the select few with a couple training spots and a massive workforce). If changes don't happen, then you need to continue reporting these violations.
It's easy for me to say at this point from an outsider's view, but it is unconscionable that SRNAs should have any priority at all compared to residents. They can sit in my room and watch from a corner, but you have given up so much and are going through hell to receive competent training. Anything other than you being the certain of attention for education is unacceptable.
Bless you for not forgetting why you became a doctor. The same four reasons everyone becomes a doctor.Don't get depressed or demoralized by the things other people are getting away with.
Being a doctor has never been about mechanical skills and procedures. Not even surgery - though obviously those skills are important.
Being a doctor is about the practice of medicine. Not just the knowledge to know how to do a procedure, but the knowledge to know when to do them, when not to do them, how to manage complications. Risks and benefits when the water is muddy. Broad and deep knowledge base to see non-obvious risks before they become dangers.
The point of being a doctor is providing the best care to our patients. The fact that some other people are doing some of the things we do, for (possibly) comparable hourly wages, after a lot less training, doesn't alter the point of being a doctor. We are what we are because we cared enough about being the best we could be, and we had the talent and drive to make it happen.
Also, chicks, money, power, and chicks.
- Joined
- Jul 21, 2014
- Messages
- 1,318
- Reaction score
- 2,781
- Points
- 5,756
- Resident [Any Field]
Did the UNC anesthesiologist issue a public statement or something? Cuz I sent in a letter too. I wasn't bashing CRNAs or anything, just saying they were woefully underqualified to take on that role, yknow, the truth. Now I'm wondering if that could possibly come back to bite me.I completely agree with your main message.
Ideally this would be good.
But realistically many PDs and Chairmen don't even have any real power to stop institutions from training future CRNAs. Nor do many attendings. Residents have even less power.
No one wants to train their replacement, but the first residents to speak out would be reprimanded and some even let go from the program. Even attendings are reprimanded. Just see what happened to Dr Elizabeth Ross at UNC for (rightly) saying what she said about CRNAs.
Maybe for this to have any real hope of success is for the vast majority of residents, attendings, PDs, Chairmen, and anyone else who wants to band together, get major media network attention, and publicly protest across the nation, even at the risk of losing their own jobs. (Similar to how junior doctors protested across the UK, though for the junior doctors nothing much really happened, not really, except now more junior doctors are trying to leave the NHS).
However, if they lose their academic jobs, where else can they go? Private groups are apparently being bought out left and right. So what's left? Locums, work for an AMC, or work for a struggling or unfair PP? Not necessarily the best options. Hence the possibility of losing their jobs would be a very real threat. Especially if they have any loans to pay back. My guess is the only ones who would be able to protest would be the ones who don't need their jobs, who have FU money saved up, which would most likely mean the older generation who are already settled in life, yet it's the older generations who are probably less likely to protest.
Otherwise, the other main solution is to let SRNAs/CRNAs train and practice completely independently. Zero support from any anesthesiologists. See how they do. But I don't know how this would realistically happen. And it's not really fair to the patients who have to suffer.
But I hope I'm completely wrong about everything I said.
- Joined
- Mar 21, 2013
- Messages
- 1,934
- Reaction score
- 2,086
- Points
- 5,271
- Resident [Any Field]
Yeah unfortunately she did have to issue a public apology. Here it is (I just copied it from the other thread):Did the UNC anesthesiologist issue a public statement or something? Cuz I sent in a letter too. I wasn't bashing CRNAs or anything, just saying they were woefully underqualified to take on that role, yknow, the truth. Now I'm wondering if that could possibly come back to bite me.
As you know, I recently submitted comments regarding the necessity of physician led anesthetic care to my United States Senator. I submitted these comments with the naïve understanding that they were private comments between myself and someone who represents me in the United States Senate. Given the nature of current political discourse, I felt compelled to use strong language to get my position across. Unfortunately, my comments were fed into the public domain. I am truly sorry that the words I chose hurt the feelings of many of you.
I want to state, without reservation, that I value all the members of our care team and that I have tremendous respect for nurse anesthetists and the important contributions they make to the anesthesia care team. However, I feel very strongly that the level of safety and quality that the team based model of care affords is superior to that proposed by current legislation and that the best level of care should be provided to every patient, particularly our nation's Veterans. My conviction is based in large part on experiences with my two grandfathers, both of whom served in the military and receive medical care in the VA system. I want my grandfathers to have the best care possible and I believe an anesthesia team benefiting from the unmatched training and education of a physician anesthesiologist is the best way to deliver that care.
I am proud to stand with my nursing colleagues at UNC in delivering exceptional anesthetic care to our patients. Unfortunately, my passion for this issue and the resultant messaging used a few words which I wish I could take back. I understand how these words could have been interpreted as calling into question the important work that you do each and every day in the care of our patients. I am sorry if you felt devalued. This was not my intent. I think we share the goal of working in an anesthesia team that provides patients the synergistic benefits of the different education and skills delivered when nurse anesthetists and physician anesthesiologists work together cooperatively.
- Joined
- Sep 8, 2008
- Messages
- 3,784
- Reaction score
- 3,783
- Points
- 5,316
- Location
- Mid-Atlantic
- Attending Physician
I know you've graduated by now, but residents really need to know that this is what the ACGME is for. There is a lot of bureaucracy and crap tied into the ACGME, but their true purpose is to ensure that training programs and producing competent physicians and the priority goes to residents within the training environment.
Fill out the survey properly and don't take any BS from your administration about losing credentialing. Most anesthesia residencies need their residents just as much as their residents need them (outside of the select few with a couple training spots and a massive workforce). If changes don't happen, then you need to continue reporting these violations.
It's easy for me to say at this point from an outsider's view, but it is unconscionable that SRNAs should have any priority at all compared to residents. They can sit in my room and watch from a corner, but you have given up so much and are going through hell to receive competent training. Anything other than you being the certain of attention for education is unacceptable.
Hard to agree with this more! The ACGME survey is incredibly important - it's anonymous, and the program has to come up with "action plans" to remedy things that have a neutral or negative evaluation (something like >40-50% neutral/negative). Some anecdotal examples from my 4 years of residency:
- Didn't have enough beds for the overnight call team, the hospital got us some bunk beds - camping style.
- Antagonistic environment up on the labor floor, particularly with male residents. Investigated, the OB residents actually had the same problem with their newer male residents. Started to be addressed when I left (at least recognizing a problem was a huge step, IMO).
- Extremely busy weekends/nights (we had a night float system) with several residents working 24+ hours straight with increasing work load requirements. Also more work over educational obligations. The program added several more voluntary moonlighting shifts to help offload the busy team.
- (Probably the most germane to this conversation): Declining reviews of teamwork in critical care (again, my program had an issue with hyper-aggressive NP fellow students but thankfully only really a problem in trauma/general surgery ICU). Solution: Slowly redistributing residents to other ICUs (cardiac ICU, vascular ICU, MICU). General surgery actually pulled all of their residents out and sent them to the VA, and there is an impending leadership change in the surgical ICUs. As for the NP fellowship program, they no longer have "minimum" procedure requirements so theoretically won't be running up and stealing procedures from residents at the last minute.
So positive change can ABSOLUTELY come from these surveys, if someone is being bullied by their program to give positive reviews that's highly inappropriate. The ACGME is incredibly clear that other learners (SRNAs, PA/NP students, etc...) are NOT to infringe upon resident education, and if they do they should be informed as such. There are definite consequences for programs that continue to have repeated issues year after year - the anesthesia program in Tampa, Florida was shut down something like 10 years ago and more recently the general surgery program in Daytona was shut as well 2-3 years ago.
- Joined
- Jan 2, 2014
- Messages
- 11,384
- Reaction score
- 24,028
- Points
- 7,061
- Location
- ヽ(´ー`)ノ
- Resident [Any Field]
Hard to agree with this more! The ACGME survey is incredibly important - it's anonymous, and the program has to come up with "action plans" to remedy things that have a neutral or negative evaluation (something like >40-50% neutral/negative). Some anecdotal examples from my 4 years of residency:
- Didn't have enough beds for the overnight call team, the hospital got us some bunk beds - camping style.
- Antagonistic environment up on the labor floor, particularly with male residents. Investigated, the OB residents actually had the same problem with their newer male residents. Started to be addressed when I left (at least recognizing a problem was a huge step, IMO).
- Extremely busy weekends/nights (we had a night float system) with several residents working 24+ hours straight with increasing work load requirements. Also more work over educational obligations. The program added several more voluntary moonlighting shifts to help offload the busy team.
- (Probably the most germane to this conversation): Declining reviews of teamwork in critical care (again, my program had an issue with hyper-aggressive NP fellow students but thankfully only really a problem in trauma/general surgery ICU). Solution: Slowly redistributing residents to other ICUs (cardiac ICU, vascular ICU, MICU). General surgery actually pulled all of their residents out and sent them to the VA, and there is an impending leadership change in the surgical ICUs. As for the NP fellowship program, they no longer have "minimum" procedure requirements so theoretically won't be running up and stealing procedures from residents at the last minute.
So positive change can ABSOLUTELY come from these surveys, if someone is being bullied by their program to give positive reviews that's highly inappropriate. The ACGME is incredibly clear that other learners (SRNAs, PA/NP students, etc...) are NOT to infringe upon resident education, and if they do they should be informed as such. There are definite consequences for programs that continue to have repeated issues year after year - the anesthesia program in Tampa, Florida was shut down something like 10 years ago and more recently the general surgery program in Daytona was shut as well 2-3 years ago.
An NP "fellow" hahaha what a joke
- Antagonistic environment up on the labor floor, particularly with male residents. Investigated, the OB residents actually had the same problem with their newer male residents. .
Whats funny is this is the complete opposite for us. Ob nurses favor the male residents and actively go after all our female residents.
OB is also off limits for crna at our place surprisingly. Yes you have to work harder on OB because of the no crna support, but we graduate with insane numbers. We get very early ob experience.
I have not even done my "official ob" month and im already well past acgme min numbers.
- Joined
- Jul 12, 2006
- Messages
- 4,755
- Reaction score
- 2,416
- Points
- 6,371
- Attending Physician
I got bored of ob after 10 epidurals...Whats funny is this is the complete opposite for us. Ob nurses favor the male residents and actively go after all our female residents.
OB is also off limits for crna at our place surprisingly. Yes you have to work harder on OB because of the no crna support, but we graduate with insane numbers. We get very early ob experience.
I have not even done my "official ob" month and im already well past acgme min numbers.
- Joined
- Jul 21, 2014
- Messages
- 1,318
- Reaction score
- 2,781
- Points
- 5,756
- Resident [Any Field]
Yeah, I kinda thought the same thing (s)he did. Good thing I'm just a pissant med student and no one cares what I think. WhewYeah unfortunately she did have to issue a public apology. Here it is (I just copied it from the other thread):
As you know, I recently submitted comments regarding the necessity of physician led anesthetic care to my United States Senator. I submitted these comments with the naïve understanding that they were private comments between myself and someone who represents me in the United States Senate. Given the nature of current political discourse, I felt compelled to use strong language to get my position across. Unfortunately, my comments were fed into the public domain. I am truly sorry that the words I chose hurt the feelings of many of you.
I want to state, without reservation, that I value all the members of our care team and that I have tremendous respect for nurse anesthetists and the important contributions they make to the anesthesia care team. However, I feel very strongly that the level of safety and quality that the team based model of care affords is superior to that proposed by current legislation and that the best level of care should be provided to every patient, particularly our nation's Veterans. My conviction is based in large part on experiences with my two grandfathers, both of whom served in the military and receive medical care in the VA system. I want my grandfathers to have the best care possible and I believe an anesthesia team benefiting from the unmatched training and education of a physician anesthesiologist is the best way to deliver that care.
I am proud to stand with my nursing colleagues at UNC in delivering exceptional anesthetic care to our patients. Unfortunately, my passion for this issue and the resultant messaging used a few words which I wish I could take back. I understand how these words could have been interpreted as calling into question the important work that you do each and every day in the care of our patients. I am sorry if you felt devalued. This was not my intent. I think we share the goal of working in an anesthesia team that provides patients the synergistic benefits of the different education and skills delivered when nurse anesthetists and physician anesthesiologists work together cooperatively.
- Joined
- Nov 24, 2007
- Messages
- 8,474
- Reaction score
- 9,828
- Points
- 7,321
- Location
- The ivory tower.
- Attending Physician
Yes.
They're doctors now too.
They do residencies.
They do fellowships.
They're equal, no, better. Because they care and trained as nurses and not cold disconnected scientists.
However our hospital has large color coded badges so a nurse will always be a nurse and a physician will remain a physician.
And I think a nurse introducing themselves as a doctor would ruffle risk management and patient safety's feathers so much here that it would end at n=1. They get worked up over far less.
--
Il Destriero
They're doctors now too.
They do residencies.
They do fellowships.
They're equal, no, better. Because they care and trained as nurses and not cold disconnected scientists.
However our hospital has large color coded badges so a nurse will always be a nurse and a physician will remain a physician.
And I think a nurse introducing themselves as a doctor would ruffle risk management and patient safety's feathers so much here that it would end at n=1. They get worked up over far less.
--
Il Destriero
- Joined
- Nov 24, 2007
- Messages
- 8,474
- Reaction score
- 9,828
- Points
- 7,321
- Location
- The ivory tower.
- Attending Physician
Oops, I forgot Board Certified.
Don't forget that.
--
Il Destriero
Don't forget that.
--
Il Destriero
The thing is the nurse practitioner has probably been doing it all day every day for years and is good at it. If it was my baby I'd rather get that person than a fellow.
don't be a douche. if everyone insisted on the most experienced person doing procedures we'd never have anyone gain experience. or do you not recall a time when you relied on the trust of strangers to learn your trade? or perhaps you don't believe in providing the same care for your patients as you would for your own family. unbelievable.
D
deleted87051
don't be a douche. if everyone insisted on the most experienced person doing procedures we'd never have anyone gain experience. or do you not recall a time when you relied on the trust of strangers to learn your trade? or perhaps you don't believe in providing the same care for your patients as you would for your own family. unbelievable.
I've seen too many CF's by trainees. That's why I don't recommend the local U for most problems to my friends and family. I have no problem being a douche in real life.
Last edited by a moderator:
D
deleted87051
flustercucks?
That would be FCs....I'm talking about CFs😉 I don't go to the barber school to get my hair cut either.
- Joined
- Jan 10, 2014
- Messages
- 247
- Reaction score
- 271
- Points
- 4,776
- Location
- Van down by the river
- Resident [Any Field]
- Joined
- Jul 28, 2011
- Messages
- 640
- Reaction score
- 303
- Points
- 5,206
- Medical Student
Jwk my favorite AA. We will try again this year to get AAs approved in my state. The dark force is strong and crafty and defeated us in committee for the bill.
We should get a bill that lays out health care naming.
What state are you in?
- Joined
- Mar 21, 2013
- Messages
- 1,934
- Reaction score
- 2,086
- Points
- 5,271
- Resident [Any Field]
"Hi. I’m Dr. Patti McCarver, and I’m your nurse."A resident or house officer is a physician (one who holds the degree of M.D., D.O., or MBBS, MBChB, or BMed) who practices medicine usually in a hospital or clinic under the direct or indirect supervision of an attending physician.
I suppose a lawsuit will be required before SRNAs quit this type of behavior. By introducing self as resident, one is directly implying "I'm a physician" and if one is a SRNA, they are not a physician. I'd be shocked if this type of behavior is legal. Worst case scenario for us, it is unethical and insulting to those who have went through medical school.
"I'm an ED doctor who's not an MD."
"When I received my doctorate I intended to introduce myself as Dr. Cash to patients and wanted staff to address me as such . . . My quest to change existing paradigms has only just begun. Wish me luck."
See threads about this here, there, everywhere!
"I admit I should have probably gone to medical school, but my opportunities for a medical degree seemed limited."
In other words, you would never have gotten in, much less survived med school. Good grief.
- Joined
- Nov 30, 2009
- Messages
- 2,011
- Reaction score
- 2,220
- Points
- 5,516
- Location
- OH
- Attending Physician
How pretentious would it be to introduce ourselves now, "Hi, I'm 0kazak1, MD", (Drop the title of Dr)
- Joined
- Dec 15, 2005
- Messages
- 17,334
- Reaction score
- 27,239
- Points
- 8,756
- Location
- Home again
- Attending Physician
Or you could say, "I'm Dr. McHugh and I'll be your physician today."
The real problem could be solved by making it illegal for anyone to introduce themselves to a patient as "doctor" when they are not a physician.
That's the case in some states, I think.
I went looking for a list the other day, when a NP introduced herself as "Dr. _______" to me after her office staff told me (several times) that "the doctor" would be with me shortly. Couldn't find a list. Still not sure if my state (Virginia) is one where it is outright illegal.
- Joined
- Jul 12, 2006
- Messages
- 4,755
- Reaction score
- 2,416
- Points
- 6,371
- Attending Physician
You guys are f***edThat's the case in some states, I think.
I went looking for a list the other day, when a NP introduced herself as "Dr. _______" to me after her office staff told me (several times) that "the doctor" would be with me shortly. Couldn't find a list. Still not sure if my state (Virginia) is one where it is outright illegal.
- Joined
- May 16, 2005
- Messages
- 401
- Reaction score
- 190
- Points
- 4,631
- Location
- The Southeast
- Attending Physician
I introduce myself as their Anesthesia Doctor. My old PD used to do the same thing and say he'd have an anesthesia nurse working with him. I like that ... anesthesia nurse. It sets the tone.
I don't have any CRNAs. AAs and Residents at my shop.
Sent from my iPhone using SDN mobile
I don't have any CRNAs. AAs and Residents at my shop.
Sent from my iPhone using SDN mobile
- Joined
- Dec 3, 2003
- Messages
- 1,750
- Reaction score
- 1,200
- Points
- 5,476
- Location
- The gamma quadrant
- Attending Physician
Fruit for the future. Check your ego at the door so what if these folks are calling themselves whatever. When it hits the fan and things get difficult you and everyone else will know who and what you are.
- Joined
- Feb 10, 2013
- Messages
- 551
- Reaction score
- 392
- Points
- 5,276
- Attending Physician
Fruit for the future. Check your ego at the door so what if these folks are calling themselves whatever. When it hits the fan and things get difficult you and everyone else will know who and what you are.
I'd rather establish right at the outset who is who.
- Joined
- Aug 25, 2009
- Messages
- 350
- Reaction score
- 390
- Points
- 5,221
- Location
- Southern California
- Attending Physician
I love to ask 'em where they went to medical school. They always glare or squirm, 100% response rate. 😀
When they are talking to me, they want to proclaim that nurses are sooo fabulous and doctors are a bunch of incompetent *****s who wasted so much time and money on medical school that they can't see straight, let alone provide anesthesia. But then when they talk to patients, they put up this smoke screen to bend over backwards and pretend they are a physician? Doesn't add up.
When they are talking to me, they want to proclaim that nurses are sooo fabulous and doctors are a bunch of incompetent *****s who wasted so much time and money on medical school that they can't see straight, let alone provide anesthesia. But then when they talk to patients, they put up this smoke screen to bend over backwards and pretend they are a physician? Doesn't add up.
- Joined
- Jun 29, 2016
- Messages
- 1,001
- Reaction score
- 1,312
- Points
- 5,526
- Attending Physician
Fruit for the future. Check your ego at the door so what if these folks are calling themselves whatever. When it hits the fan and things get difficult you and everyone else will know who and what you are.
It's not about ego, it's about protecting your profession. You give an inch and they take a mile. What's to say in the future when everyone thinks they are doctors, and start saving the day themselves without you. Who needs two doctors when there already is one (not you)
- Joined
- Jun 26, 2008
- Messages
- 1,827
- Reaction score
- 3,003
- Points
- 5,791
- Attending Physician
Fruit for the future. Check your ego at the door so what if these folks are calling themselves whatever. When it hits the fan and things get difficult you and everyone else will know who and what you are.
Not even about ego. It's about the further blurring of lines between physicians and non physicians. Everyone wants the respect, pay, and authority of a physician without actually being a physician or going through what we go through to get the actual title of physician.
Short term it's just the title. Long term it is going to be about the pay and control. The more these lines get blurred now, the worse it will get in the future.
- Joined
- Dec 5, 2013
- Messages
- 908
- Reaction score
- 809
- Points
- 5,171
- Attending Physician
Yep, I post about it a lot but my shop had an NP critical care fellowship. They often introduce themselves as ICU (nursing) fellows. Really glad I don't work there anymore, they were exceedingly aggressive and nasty towards residents/real fellows.
My upcoming PP job apparently has SRNA rotators at a couple sites, if any of them introduce themselves as a "nurse anesthesia resident" to me I'll probably just laugh.
Why in private practice would you voluntarily train people who want to take your job, and who says they do as good a job at it? Anesthesia is the only field that seems to aggressively try to replace themselves.
- Joined
- Nov 24, 2007
- Messages
- 8,474
- Reaction score
- 9,828
- Points
- 7,321
- Location
- The ivory tower.
- Attending Physician
Why in private practice would you voluntarily train people who want to take your job, and who says they do as good a job at it? Anesthesia is the only field that seems to aggressively try to replace themselves.
Money.
--
Il Destriero
- Joined
- Feb 10, 2013
- Messages
- 551
- Reaction score
- 392
- Points
- 5,276
- Attending Physician
Money.
--
Il Destriero
A few years ago when I was chairman of my group (we rotate the post), I got a phone call from a Srna program in north Chicago asking if we would be interested in training srnas. My answer was 'not just No, **** No!'
Similar threads
- Replies
- 36
- Views
- 4K
- Replies
- 218
- Views
- 15K
