The only reason I'm replying is to make sure to stamp out the fake news.
This is comparing against peak prostate cancer diagnoses thanks to the advent of PSA testing. Our center and other centers have recently been seeing increasing demand for prostate cancer RT.
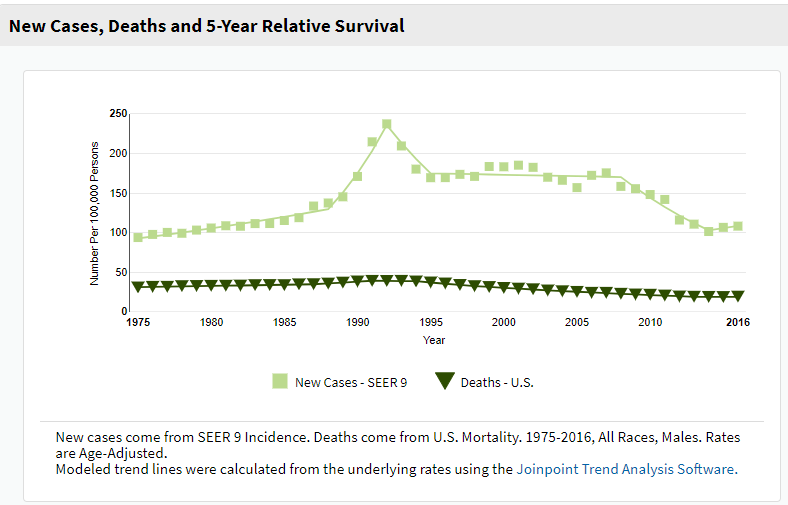
So how do you think this is possible. Prostate cancer is, as you know, the most common cancer in men. Number of new cases per year has dropped by
~33% over the last 10y, and we are about
25y out from the advent of PSA testing. The incidence held steady as you can see for many years after this advent (1990-95 time frame).
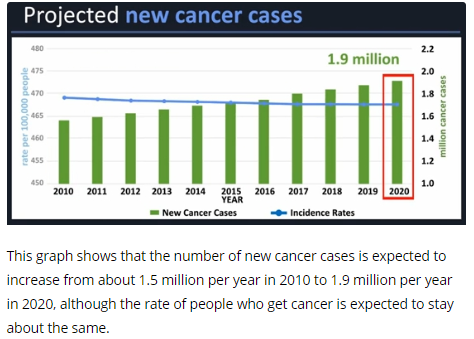
Other estimates from better-regarded sources, as I’ve discussed before, actually predict an increase in cancer incidence overall.
"Better-regarded sources" is
weasel wording and a
logical fallacy. Who's predicting this increased incidence in the U.S.? Smoking is on the downswing thus lung CA decreasing, prostate CA trends as noted above. You have previously cited
one source which says the number of
incident cases will increase in America by <1 million over the next 20 years and this will
thus equal a ~1% rise in
incidence per year. Surely you can realize that if this one single source's modeling is even mildly off... and follows the
recent trend...
... incidence may flatline or decrease.*
current residents would agree with me that someone’s prior claim that MGH treats something like 8 lung SBRTs per year reflects a shockingly low number.
I will call you out for weasel wording again ("would agree with me"... that's nice!), and that "someone" is me. And it wasn't a claim. I was
simply citing a
source which revealed that at a lung nodule clinic at MGH they saw about 140 patients/year which yielded about 8 lung SBRTs a year. Draw conclusions from that as you will. But I have also cited
national data showing that over a 10y period about 30,000 (out of ~150,000) patients at most got lung SBRT which translates to about 3,000 cases per year. We can be very confident that no more than ~15,000 patients per year are getting lung ca SBRT in the U.S.
This number is where I get the ~3 lung SBRTs for every rad onc in America (on average) metric.
Just trying to introduce a dose of reality!
Back to your "better-regarded sources" and my "claims." Hopefully I have not made any "claims" per se. And my sources here were SEER, the CDC, The Oncologist, the JNCI, and the Red Journal. And a few random internet links for fun. However you have made claims which are, from my end, impossible to falsify. This does give you the virtue of never being provably wrong.
*even the CDC's 2015 modeling was off. They predicted ~1.9 million cases for 2020 in 2015. But now that we are five years in the future from 2015, and actually in 2020, we can better see the actual 2020 number will be about ~1.8 million for 2020. About 5% less than what the CDC predicted just 5y ago.