- Joined
- Oct 4, 2017
- Messages
- 5,016
- Reaction score
- 9,782
We refused to put pts on her anal trial because volumes were idiotic.Talk about falling up.
We refused to put pts on her anal trial because volumes were idiotic.Talk about falling up.
We refused to put pts on her anal trial because volumes were idiotic.
Multiple chairs in the last decade. Not really known for good education, also home to an exploitative unaccredited fellowship. They love cheap resident and fellow laborcan you clarify why columbia is terrible? also why kachinic is bad?
Just 2 right? They didn't have a chair for >half the decade & took awhile to recruit one. Department is small and I don't see how it could support 8 residents (not to mention an occasional fellow)Multiple chairs in the last decade. Not really known for good education, also home to an exploitative unaccredited fellowship. They love cheap resident and fellow labor
can you refresh our memoriesWe refused to put pts on her anal trial because volumes were idiotic.
Who treats elective volumes at 1.5/day?can you refresh our memories
I was in a conversation about the creation of that trial. Apparently the doses and volumes were created "by committee", with some of the committee members insisting on large, old-school volumes that made it into the final cut. Not everyone agreed with them, but it was the only way to get consensus among the panel.We refused to put pts on her anal trial because volumes were idiotic.
huge margins so that not much of difference between imrt and 2dcan you refresh our memories
I was in a conversation about the creation of that trial. Apparently the doses and volumes were created "by committee", with some of the committee members insisting on large, old-school volumes that made it into the final cut. Not everyone agreed with them, but it was the only way to get consensus among the panel.
Just 2 right? They didn't have a chair for >half the decade & took awhile to recruit one. Department is small and I don't see how it could support 8 residents (not to mention an occasional fellow)
Since (despite what some people say or think) there is no neural tissue residing in the balls—and thus balls are incapable of independent, intelligent thought— yes, it's ballsy.Seems like there are at least 11 attendings, although I'm not sure how many of those are main campus vs satellites.
Regardless, in the current climate, to EXPAND a residency program, while incredibly short-sighted and selfish, is definitely real ballsy.
Those taiwanese mafia scandals will get you.In regards to Columbia Rad Onc, I think the recent chairs were something like this:
Clifford Cao 2008 to 2015? had to resign due to some conflict of interest scandal in Taiwan.
Silvia Formenti 2015 to ? Chair of joint Cornell/Columbia program?
Lawrence Schwartz 2018? Interim chair (but is the chair of radiology)
Lisa Kachnic 2019 to present.
Has there been actual confirmation of this?Seems like there are at least 11 attendings, although I'm not sure how many of those are main campus vs satellites.
Regardless, in the current climate, to EXPAND a residency program, while incredibly short-sighted and selfish, is definitely real ballsy.
Rumor was that he was just horrible and rarely present.Those taiwanese mafia scandals will get you.
He did have that cliff chao book which allowed many old timers to learn IMRTRumor was that he was just horrible and rarely present.
Seems like there are at least 11 attendings, although I'm not sure how many of those are main campus vs satellites.
Regardless, in the current climate, to EXPAND a residency program, while incredibly short-sighted and selfish, is definitely real ballsy.
Simplify? YesCan someone simplify this discussion? Oversaturation? Too many residents?
Physics job market is very good right now, esp with experience and BC, even in places where the rad onc job market is terribleSimplify? Yes
Don't do it. Hands down better control of the specialty in Med Physics. Covid will hurt for a bit but that hurts everyone in healthcare. Physicists are the least harmed by fractionation or reimbursement changes. And there is much less incentive to increase residencies in their case because they cost money.
But then again..... that means that physicist residents save money? (foreshadowing......)
Physics job market is very good right now, esp with experience and BC, even in places where the rad onc job market is terrible
I believe the physicist at my last rural gig did 15 minutes of "actual work" per week.Physics job market is very good right now, esp with experience and BC, even in places where the rad onc job market is terrible
On the other hand, the market for therapists looks even bleaker than rad onc physicians. The therapy programs are pumping those guys out like crazy and fractionation will affect them the most.There will always be a market for good physicists
I still rather have extra therapists around then a RN. I think a resident would be the gold standard.On the other hand, the market for therapists looks even bleaker than rad onc physicians. The therapy programs are pumping those guys out like crazy and fractionation will affect them the most.
I still rather have extra therapists around then a RN. I think a resident would be the gold standard.
To be honest I work in a hospital that has residents rotate in our dept... never ever let your attending have you believe a resident isn’t useful to them. I can get more out of a pgy-1 psych resident then I can my nurse who has been working here for over 20 years!
Yup...in the same way an ICU nurse is better than an intern on the unit. People get better with years and years of experienceYo that sucks. My nurses, honestly, are better than a PGY-2 or 3 resident.
As someone who started residency long after IMRT was "the norm", this trial (and anal cancer in general) was really how I came to understand and appreciate what people are comfortable with (margins) and how what decade (and where) they trained influenced that comfort.
So, I at least appreciate 0529 as "how I learned to contextualize studies and techniques"?
But...I don't think that was the intent...
Sounds like a good trial for protons!
Anal proton plans can look very niceSounds like a good trial for protons!
I think UCincy is enrolling.
In my experience with some patients treated with protons (not by me, but by colleagues), the perineal skin reaction is even worse. It's true of breast cancer so it seems it would be true of anal as well. I bet the bowel toxicity might be better though (depending on your volumes).
For some reason. I would have figured you would be more into this modality:Anal proton plans can look very nice
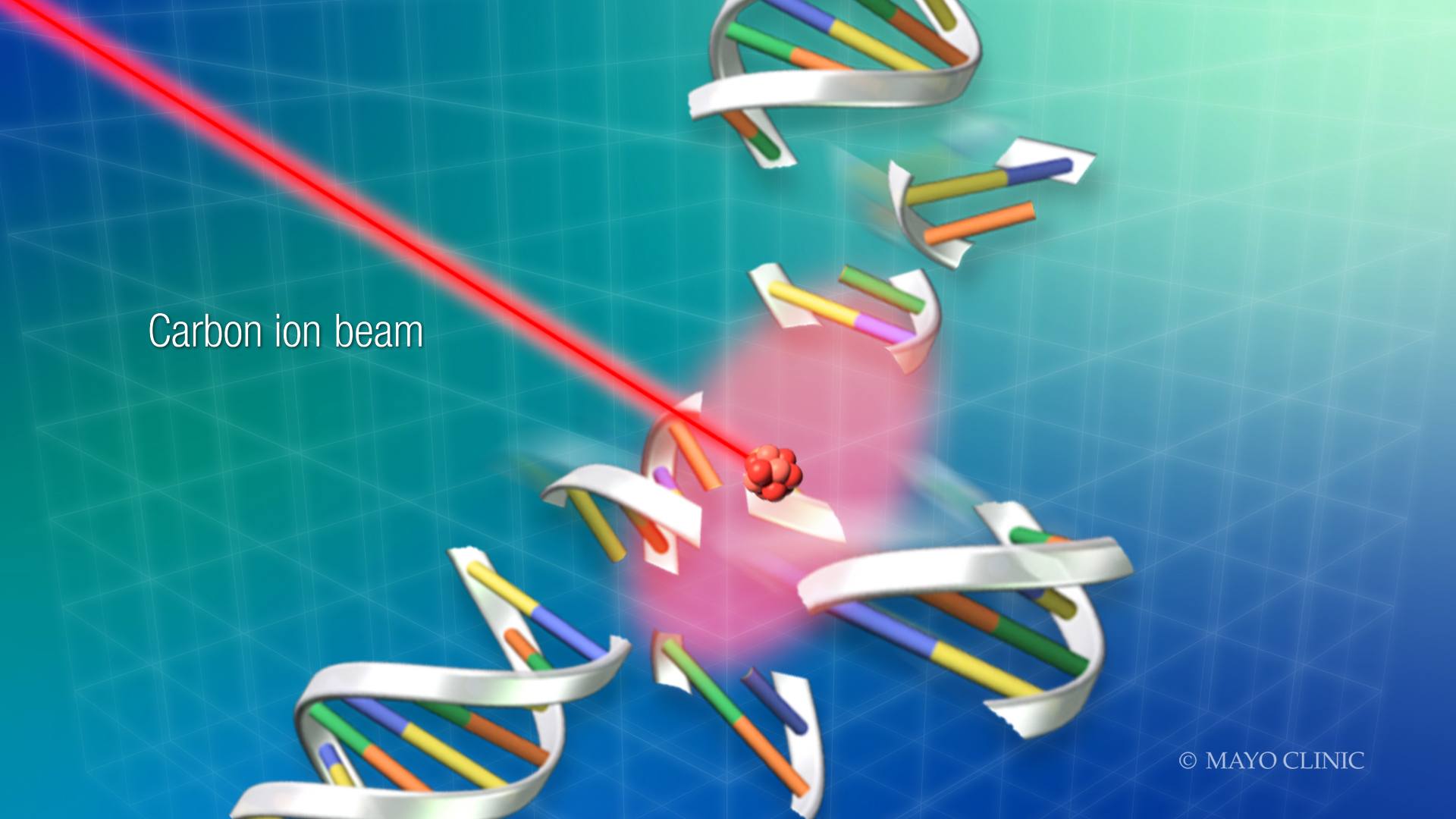
You would want the proton or carbon plan if you had anal cancer. You know you would.For some reason. I would have figured you would be more into this modality:
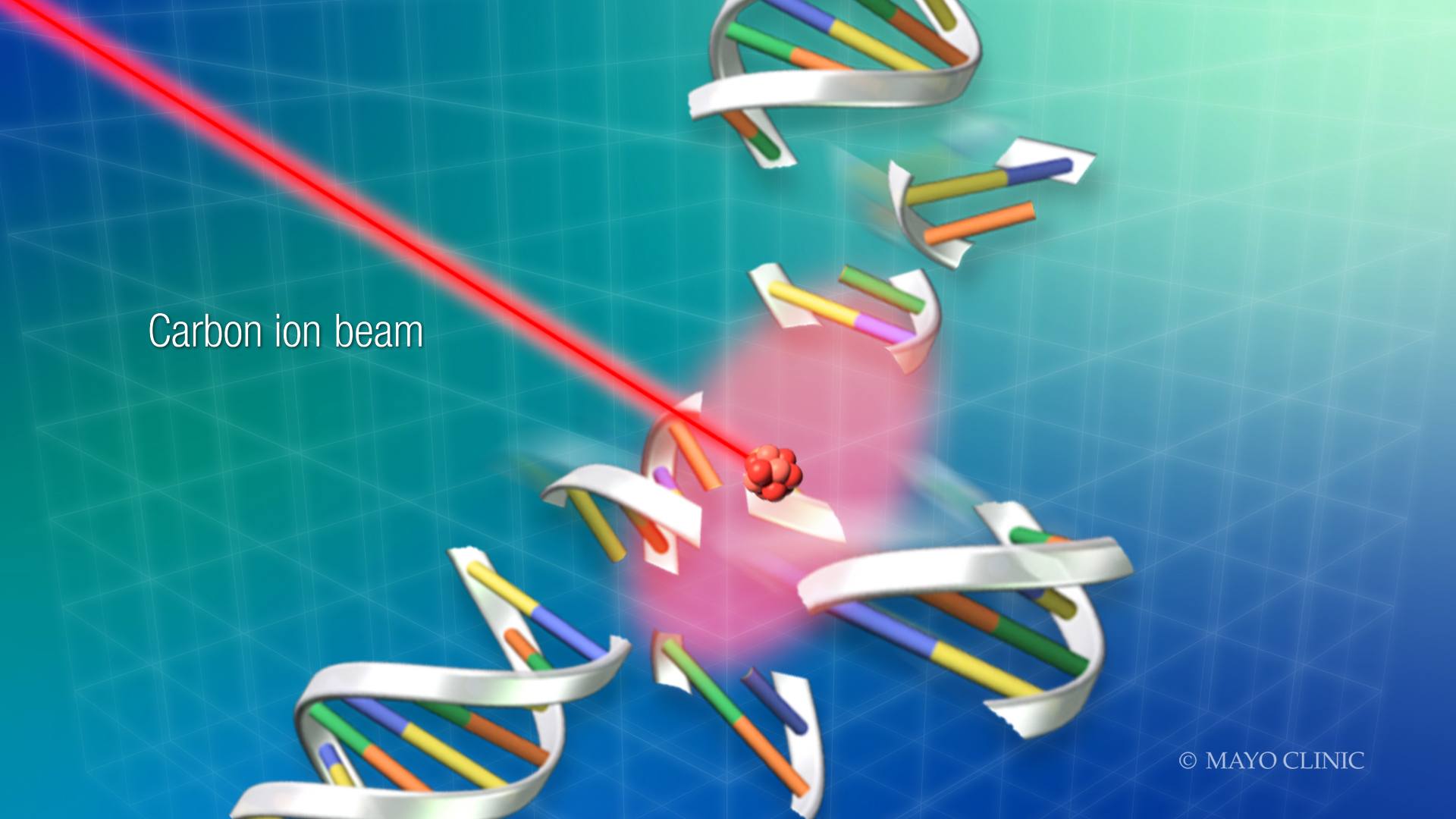
Mayo Clinic, Hitachi to build first, next generation, carbon ion therapy treatment facility in North America - Mayo Clinic News Network
ROCHESTER, Minn. and TOKYO, Japan — Mayo Clinic and Hitachi, Ltd. have reached an agreement in principle to build a carbon ion treatment facility as part of Mayo Clinic's recently announced integrated oncology facility which will be constructed at Mayo Clinic's campus in Jacksonville, Florida...newsnetwork.mayoclinic.org
Agree with what everyone is doing, no reason to stick with such ridiculous fractionations when you can extrapolate doses from other disease sites.
Last I checked it’s pretty much all we got that’s “new” in regards to radiation and anal cancer. That should also be a sign of where we are today.Criticizing 0529 design and methods... What year is this again
All I know is that I definitely don’t want a “boost” in my anus.You would want the proton or carbon plan if you had anal cancer. You know you would.
Lol.All I know is that I definitely don’t want a “boost” in my anus.
You know what you like!All I know is that I definitely don’t want a “boost” in my anus.
All I know is that I definitely don’t want a “boost” in my anus.
I heard they were trying to double the number of residents from 6 to 12. Any increase in this climate obviously is absurd and reflects a complete disregard for residents, non-boomer attendings, and the general future of this field. So irresponsible and selfish.Just 2 right? They didn't have a chair for >half the decade & took awhile to recruit one. Department is small and I don't see how it could support 8 residents (not to mention an occasional fellow)
Well, programs with 6 or fewer residents were the problem according to Kachnic when she and the ABR failed half a class. Increasing it to 12 makes her part of the solution, clearly.I heard they were trying to double the number of residents from 6 to 12. Any increase in this climate obviously is absurd and reflects a complete disregard for residents, non-boomer attendings, and the general future of this field. So irresponsible and selfish.
Could you extrapolate on why you would discourage anyone from medicine? I'm about to apply to med school next year and thats all I hear.1) It's actually more due to the change in standard of care for breast and prostate, the most common cancers treated by Radiation Oncology. Breast used to always be like 25 fractions, prostate like 44. Now breast is ~15 and prostate is ~28 (again, grossly over simplifying). SRS/SBRT plays a part, but you could argue that helps us treat more patients than we were 20 years ago (Stage I lung or oligomets, for example). There are multiple other examples as well (active surveillance for low risk prostate etc).
2) RadOnc or not, I would absolutely not recommend going to medical school - it's not a good investment in yourself. This conversation can go in 1,000 different ways, and I'm sure people will disagree with me about this...but I will be actively discouraging my children from going into medicine.
Are you already a board-certified medical physicist or are you still in training?
FAANG/techCould you extrapolate on why you would discourage anyone from medicine?
Could you extrapolate on why you would discourage anyone from medicine? I'm about to apply to med school next year and thats all I hear.
Sounds like Pathology!!!!Congratulations, only 109 Rad onc MD applicants this year; with total 176 applicants. Soon Rad onc will be an escape for those who didn't match in the SOAP, and a guaranteed visa for FMGs that want to move to the United States.
Grad Type ERAS 2016 ERAS 2017 ERAS 2018 ERAS 2019 ERAS 2020 ERAS 2021
DO 10 3 9 8 10 16 IMG 44 38 19 30 40 51 MD 215 233 213 183 143 109
