- Joined
- Dec 26, 2006
- Messages
- 7,313
- Reaction score
- 20,116
- Points
- 9,596
- Attending Physician
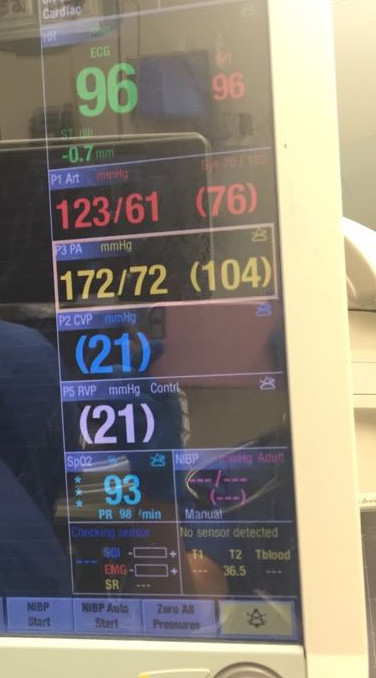
That's true, but then the OP must have gotten the PASP from a RHC and not from Bernoulli's equation on echocardiography. Otherwise the TR Vmax to calculate an RVSP that high would show a decent degree of TR
Not necessarily. TR vmax and MR vmax have very little to do with the true degree of TR and MR (you'll notice that TR and MR vmax are not part of ASE classification of valvular regurgitation). If anything, when you have severe TR the vmax will decrease as there is now a very small gradient between the two chambers because there is so much communicating flow. For instance, it's not uncommon to have a very high CVP of 35 and a RVSP of 45 with wide open TR. The TR is quite severe but the gradient between the RA and RV is pretty low. As the RV dilates out and function worsens, the TR vmax may go even lower as having poor systolic function will further lower the peak regurgitant velocities.