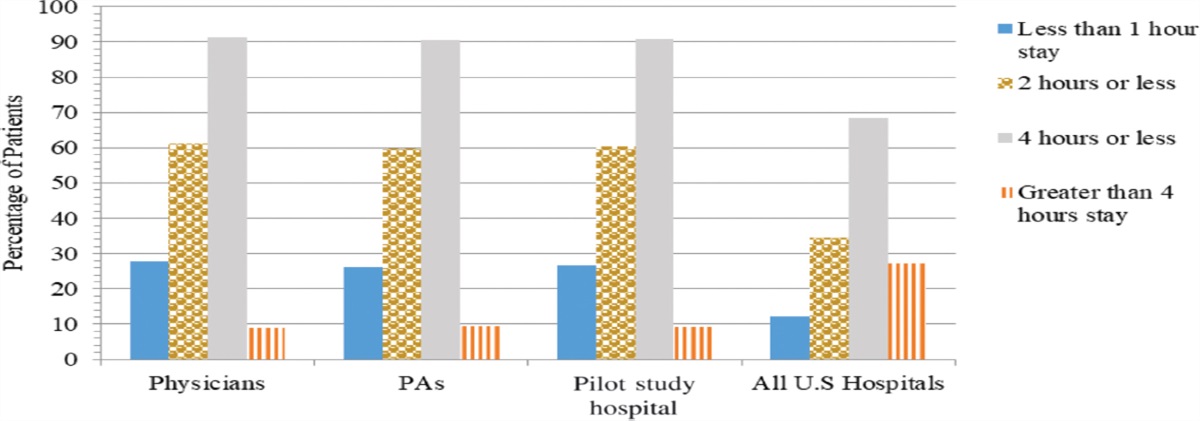
f the host institution were analyzed. Although minor variances in metrics were appreciated, transfers, 72-hour returns, and death rates were all similar among provider types. Results from this work do not demonstrate a clinically meaningful difference among ED metrics between physicians and PAs...
journals.lww.com
Just came off shift where I worked alongside an EM doc a few years out of 3 year residency. Last patient with pneumonia failing bipap with hypercapbeic failure. Elderly, obese, COPD on 5 L at home, multiple neck surgeries on what little neck there was, kyphotic, malampatti 3. Looked like a terrible intubation. Did DSI with ketamine and when we laid pt back the neck was stiff as a board with neck locked in flexion. Just a terrible situation.
Doc got that tube so smoothly it was just amazing. Made it look easy. Got it in about 3 seconds.
I'm confident I could have gotten it too. Would have taken longer. I would have "ticked" down the tongue instead of just inserting to just the right depth and position....but I'm confident I would have gotten it.
Would the outcome have been different had I been single coverage? I dunno.
In my experience there is an obvious difference in how EM trained docs think and practice. But how much of a difference does this make with actual outcomes? There HAS to be a point of diminishing returns with training (are 4 year EM residencies better than 3? What's the NNT?) Are EM docs over trained for what they do?
What is the NNT to show an improved outcome for an EM trained doc over a non-em trained doc, or over an experienced EM PA, or a fresh PA, or a nurse....