I am an almost graduated senior with a bs in biology and psychology trying to decide between medical school for psychiatry (possibly child and adolescent) or grad school for clinical psychology. If grad school, I would prefer the psyD route since I'm more interested in clinical practice than research, however I am aware of the limitations in terms of funding and the number of years needed to obtain the psyD. I took my MCAT in August but started having doubts about my desire to go to medical school. I'd have yet to apply to either med school or grad school but am planning on taking a year off to do related work and/or Americorps. I have a 3.6 GPA and 509 (I think equivalent to 31 or 32 on older version) on MCAT. Knowing this info, does anyone have any advice or strong preference for which route I should take? Thanks so much.
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Medical school vs graduate school decision
- Thread starter Art127
- Start date
- Joined
- Feb 15, 2009
- Messages
- 18,026
- Reaction score
- 23,767
There's a few of these threads in the archive, I'd suggest a quick search of those. Couple of quick points.
1. Very different career trajectories and career responsibilities between these two. Depends on how you see your day to day responsibilities.
2. The notion that a PhD is all about research is an outdated notion and has not been accurate for a few decades now. Also many threads that discuss this.
1. Very different career trajectories and career responsibilities between these two. Depends on how you see your day to day responsibilities.
2. The notion that a PhD is all about research is an outdated notion and has not been accurate for a few decades now. Also many threads that discuss this.
- Joined
- Dec 18, 2005
- Messages
- 5,136
- Reaction score
- 8,194
Go to medical school: there is higher employment, higher pay, greater portability of career, and greater ability to make a lateral career move.
Would people agree that M.D takes quite a bit more commitment than Phd? Obv Phd students have to work really really hard (I'm sure between 40-60hrs) a week, but I don't think anything can really match clinical rotations and residency to get the M.D.
Last edited:
- Joined
- Feb 15, 2009
- Messages
- 18,026
- Reaction score
- 23,767
Depends on specialty. For example, neuro. 5 years grad school, 1 year internship, 2 year postdoc. I think they both take a ton of commitment, just depends on what type of commitment you're looking for.
There's a few of these threads in the archive, I'd suggest a quick search of those. Couple of quick points.
1. Very different career trajectories and career responsibilities between these two. Depends on how you see your day to day responsibilities.
2. The notion that a PhD is all about research is an outdated notion and has not been accurate for a few decades now. Also many threads that discuss this.
Thanks for the advice! I know that there are PhD programs where there is less emphasis on research but still research none the less. I just am unsure if conducting research in general is really for me...But I will definitely explore threads on this.
- Joined
- Feb 15, 2009
- Messages
- 18,026
- Reaction score
- 23,767
Thanks for the advice! I know that there are PhD programs where there is less emphasis on research but still research none the less. I just am unsure if conducting research in general is really for me...But I will definitely explore threads on this.
Many programs are more balanced, with a good portion of those offering more clinical than research. A solid research background is essential in being a psychologist, though. Far too many providers with little to no understanding of what they are doing when it comes to evaluating research findings.
- Joined
- Mar 24, 2014
- Messages
- 5,527
- Reaction score
- 6,556
Expertise in research methodology and the critical thinking skills involved in this is part of what makes a psychologist. Expertise in medicine is part of what goes into being a psychiatrist. Psychiatry pays 2 to 3 times as much. Both paths are challenging.
- Joined
- Jan 7, 2010
- Messages
- 9,319
- Reaction score
- 5,585
Would people agree that M.D takes quite a bit more commitment than Phd? Obv Phd students have to work really really hard (I'm sure between 40-60hrs) a week, but I don't think anything can really match clinical rotations and residency to get the M.D.
(My) short answer--no. Different types of commitment and emphasis on different skills, but not less of either.
If we're talking the raw amount of information expected to be learned, the first two years of med school win out. Hours, could be a wash. Psych grad students aren't pulling repeated 36-hour hospital shifts or seeing 10,000 pts by the time they finish. Conversely, they're involved in continual self-directed long days and all-nighters when you're "off the clock" (because in grad school, there really is no clock).
- Joined
- Dec 18, 2005
- Messages
- 5,136
- Reaction score
- 8,194
Would people agree that M.D takes quite a bit more commitment than Phd? Obv Phd students have to work really really hard (I'm sure between 40-60hrs) a week, but I don't think anything can really match clinical rotations and residency to get the M.D.
Length of training: Mildly. PsyD/phD has around a median time to complete of 5.4 years. But even after you complete your degree you are required to complete an at least one year post doc to get licensed. So 6.4 years or so. Median income is around 88k. Compared to an md with a median completion of 4 years, plus 3 of residency. So 6.4 years vs 7. If you add in a speciality such as neuropsych, forensics, or medical psych the training becomes longer.
Residency: Next you might say "well residency is super intense". Yeah, look on the psychology Sdn boards. You'll see people indicating a minimum of 50hr weekend, with many reporting 60-80 hrs. So maybe slightly lower hours for residency, and for a shorter period of time. Oh yeah, we get paid about 40% of medicine resident salaries.
Rotations: As for rotations, we call them practica or externships, and yes we do them. Iirc the minimum is 20/hrs a week, for two years. If you read the board many put in more hours with writing reports from home in addition to the face to face hours. As you'd expect, the "20hrs minimum" is interpreted by some attendings as "how much scut work can I get out of this kid" while some adhere to the hours. There is traditionally an opportunity for another year long rotation in year three. Because match uses hours for stats, it is in ones best interest to do this in addition to applying to match, interviewing, and completing dissertation.
Match: yeah we use or at least used to use the exact same program as medicine for match, with the traveling for interviews, and having a computer algorithm telling us where we are going to live next year.
Post doc: now you have all your degrees, but you are not licensed! Awesome. Unless you want to go back to stripping, you either have to participate in a post doc match or find your own. People get paid less than medical residents again, around 35-45k/yr.
Post licensure: you're done! Start looking for jobs. Notice how few there are? Compare that to a physicians recruiter, which is funny because recruiters almost don't exist for psychologists. Do yourself a favor and Google physician positions for one location vs psychologist positions for the same location.
Money: duh.
D
deleted343839
Would people agree that M.D takes quite a bit more commitment than Phd? Obv Phd students have to work really really hard (I'm sure between 40-60hrs) a week, but I don't think anything can really match clinical rotations and residency to get the M.D.
They are different types of commitment. Success in graduate school really hinges on self direction and independent thinking (balanced with good use of mentoring/supervision). Success in medical school is more performance-based, and the training is more structured.
Sent from my iPhone using Tapatalk
Thanks for all the responses! Another question: I spoke with a forensic psychiatrist and she said that psychiatrists aren't as likely to do actual therapy with patients, partly due to it being frowned upon by someone more qualified such as a psychologist. What are thoughts on this? If I go the med school path I'd like to be able to prescribe meds but also would like to possibly do therapeutic treatment with my patients as well. That was just one psychiatrists opinion so I'm curious to know other views.
- Joined
- Jan 7, 2010
- Messages
- 9,319
- Reaction score
- 5,585
Thanks for all the responses! Another question: I spoke with a forensic psychiatrist and she said that psychiatrists aren't as likely to do actual therapy with patients, partly due to it being frowned upon by someone more qualified such as a psychologist. What are thoughts on this? If I go the med school path I'd like to be able to prescribe meds but also would like to possibly do therapeutic treatment with my patients as well. That was just one psychiatrists opinion so I'm curious to know other views.
Psychiatrists get training in psychotherapy while on residency, although per psychiatrists on SDN and elsewhere, the quality and depth of that training varies widely between sites.
If you want to conduct psychotherapy, you certainly can. But if you're an employee rather than your own boss, the opportunities may be limited, in no small part because medical management reimburses better (and unlike psychotherapy, psychologists and LCSWs can't do it). Although given the shortage of psychiatrists in the community, if you made your hiring contingent upon being afforded at least some opportunity to perform psychotherapy, I'd imagine many/most employers would be receptive, within reason. The SDN psychiatry section can provide more information on this, though, and there are threads over there you could browse related to folks having this same question.
- Joined
- Apr 6, 2007
- Messages
- 10,827
- Reaction score
- 5,609
Thanks for the advice! I know that there are PhD programs where there is less emphasis on research but still research none the less.
This should rule-out the field ad profession of clinical psychology for you then. This attitude would led itself to research based education/training/field.
Medicine will require learning a but loaf of basic science of course, but a desire and ability for research competence is more fundamental to the skill set of a psychologist, both because of the type of constructs, variables, phenomena, assesment and treatments we do and because jobs will expect you to be able to bring this skill to the table in varying forms.
- Joined
- Jul 17, 2014
- Messages
- 181
- Reaction score
- 177
I think this is misinformation. It is true that some jobs for clinical psychologists are designed for people with the ability and desire to conduct research. However, these days the line between doctoral level and master's level is fuzzy, and many job listings reflect this. I'm not saying this is a good thing but I do think it's a reality. It's actually somewhat hard to find jobs with a balance of clinical and research duties.
I do think one should stay away from doctoral training if they have no desire to spend 5 years pretending to like research.
I do think one should stay away from doctoral training if they have no desire to spend 5 years pretending to like research.
An article about med school. I think you guys are under-estimating the toll med school takes on people. I honestly think it's not something you can get through unless you are absolutely certain it's something you want. Working 36-48hrs in a row, nights, over 100hrs easily/week etc is brutal.
http://www.theglobeandmail.com/glob...brightest-and-the-burned-out/article19179842/
http://www.theglobeandmail.com/glob...brightest-and-the-burned-out/article19179842/
- Joined
- Mar 24, 2014
- Messages
- 5,527
- Reaction score
- 6,556
It is my understanding that the long hours are during residency, not during med school and that psychiatry residencies tend to be more reasonable in their demands on their residents. The psychiatry forums talk about some programs that might work you more than others, but it ain't surgery.An article about med school. I think you guys are under-estimating the toll med school takes on people. I honestly think it's not something you can get through unless you are absolutely certain it's something you want. Working 36-48hrs in a row, nights, over 100hrs easily/week etc is brutal.
http://www.theglobeandmail.com/glob...brightest-and-the-burned-out/article19179842/
If one's goals are purely clinical, I'd generally recommend medical school. I think the main advantage of psychology are in things that do not directly relate to patient care (research, program evaluation/outcome assessment, etc.). The approaches can certainly be different, but I think there is enough overlap that one can usually carve out the desired career and utilize their desired approach in either field if truly desired. That said, you'll often hear the phrase "Physician first, psychiatrist second" here so if you aren't interested in all the other things that go along with medicine, medical school is going to be a nightmare.
I don't know that its necessarily hard to find jobs that blend clinical and research activities, it just depends on where you are looking, what types of positions you are looking and what your qualifications are. For instance, most AMCs/VAs seem to expect at least some level of research involvement, even from folks on clinical tracks (though obviously the extent of this can vary tremendously). I think the problem is that this is one area where we differentiate ourselves so the jobs that blend doctoral and master's level training often come with even lower pay (generalization - obviously not true in all cases).
I don't know that its necessarily hard to find jobs that blend clinical and research activities, it just depends on where you are looking, what types of positions you are looking and what your qualifications are. For instance, most AMCs/VAs seem to expect at least some level of research involvement, even from folks on clinical tracks (though obviously the extent of this can vary tremendously). I think the problem is that this is one area where we differentiate ourselves so the jobs that blend doctoral and master's level training often come with even lower pay (generalization - obviously not true in all cases).
- Joined
- Jan 7, 2010
- Messages
- 9,319
- Reaction score
- 5,585
An article about med school. I think you guys are under-estimating the toll med school takes on people. I honestly think it's not something you can get through unless you are absolutely certain it's something you want. Working 36-48hrs in a row, nights, over 100hrs easily/week etc is brutal.
http://www.theglobeandmail.com/glob...brightest-and-the-burned-out/article19179842/
I don't think folks are underestimating the toll med school can take on a person; it's an exceedingly difficult path to follow. I do think folks tend to underestimate the toll grad school can take, and this is also likely more variable from advisor to advisor and program to program than is the case with medical school.
That being the case, I also think there are folks who go into medicine for a variety of reasons that may later falter (e.g., prestige, money, to prove they can because it's so difficult). There may not be quite as many of these in psych grad school programs because both the money and prestige typically associated with the positions aren't that of a physician. Thus, more med than psych grad students may be prone to burning out and/or becoming disillusioned. Although proportionally, I don't know if this is the case (i.e., plenty of folks drop out of grad programs within the first few years).
Edit: And agreed with both Ollie and erg. If the research interests truly are minimal or nonexistent (i.e., not necessarily conducting research oneself after training, but even just being exposed to methodologies, conducting research while in grad school, and staying "up" on these factors after graduating), and med school is an option, I'd likely recommend you go that route. I personally love what I do, but physicians certainly get paid much more on average, and have an easier time finding jobs regardless of the location.
Last edited:
Well even 3rd-4th year of med school will require you to do rotations, so ya you will have easier rotations but also have to do emergency medicine, pediatrics, obgyn, etc that will certainly be challenging and you'll have to be on call (after working long hours). Then yes, residency will be much worse. lolIt is my understanding that the long hours are during residency, not during med school and that psychiatry residencies tend to be more reasonable in their demands on their residents. The psychiatry forums talk about some programs that might work you more than others, but it ain't surgery.
- Joined
- Apr 6, 2007
- Messages
- 10,827
- Reaction score
- 5,609
I think this is misinformation. It is true that some jobs for clinical psychologists are designed for people with the ability and desire to conduct research. However, these days the line between doctoral level and master's level is fuzzy, and many job listings reflect this. I'm not saying this is a good thing but I do think it's a reality. It's actually somewhat hard to find jobs with a balance of clinical and research duties.
I do think one should stay away from doctoral training if they have no desire to spend 5 years pretending to like research.
ALL jobs blend the two. That's your job as scientist-clinician.
Many jobs outside private practice will also have some degree or role in which research competency/knowledge in varying forms will be used, or will be expected to be used. I have a 100% clinical job (sans the 4 hours per week as assistant director of clinical training) and "Scholarly Productivity" is on my yearly performance evaluation.
Last edited:
- Joined
- Jul 17, 2014
- Messages
- 181
- Reaction score
- 177
Scientist-clinician is only one type of training model. One may dislike the scholar-practitioner model, but it's now firmly entrenched in our field, and I believe the reality of the job market bears this out. I have seen plenty of colleagues from strong scientist-practitioner model PhD programs accept clinical positions with no research responsibilities.
- Joined
- Apr 6, 2007
- Messages
- 10,827
- Reaction score
- 5,609
Scientist-clinician is only one type of training model. One may dislike the scholar-practitioner model, but it's now firmly entrenched in our field, and I believe the reality of the job market bears this out. I have seen plenty of colleagues from strong scientist-practitioner model PhD programs accept clinical positions with no research responsibilities.
I think we are using different operational definitions of "research."
- Joined
- Jul 17, 2014
- Messages
- 181
- Reaction score
- 177
Could be. I think a psychologist needs to understand that every intervention should have an empirical basis. I don't think the majority of psychologists conduct research once they are out of school.
These things might be obvious to us, but to someone considering a career in psychology vs. medicine, it might not be obvious.
I agree that people underestimate how difficult psychology grad school is.
These things might be obvious to us, but to someone considering a career in psychology vs. medicine, it might not be obvious.
I agree that people underestimate how difficult psychology grad school is.
- Joined
- Feb 15, 2009
- Messages
- 18,026
- Reaction score
- 23,767
I think he was more commenting on the aspect that one needs a solid research foundation to understand the research behind the intervention they are doing. And, also be able to critically evaluate new research that comes out so that they may refine their approaches along their careers to coincide with best practices. Otherwise, we get people doing qEEG, recommending Aricept, or continuing to do psychoanalysis.
- Joined
- Jul 17, 2014
- Messages
- 181
- Reaction score
- 177
Agreed. I've had recent trouble trying to help patients who had been indoctrinated by an Internal Family Systems therapist. Still trying to find quality research on that one.
- Joined
- Apr 6, 2007
- Messages
- 10,827
- Reaction score
- 5,609
What's the intervention where you tell anxious or depressed patient to tap on their face? I had some of this nonsense yesterday...
I do this when I have impacted sinuses, I guess it does make me feel I'm doing something for it.
I do this when I have impacted sinuses, I guess it does make me feel I'm doing something for it.
- Joined
- Dec 18, 2005
- Messages
- 5,136
- Reaction score
- 8,194
Otherwise, we get people doing qEEG, recommending Aricept, or continuing to do psychoanalysis.
Aricept: There was an article about 10 years ago about what patient's families want to know when getting diagnosed with dementias. IIRC, it was titled something like "the rule of three" with diagnosis, prognosis, and possible interventions being the three. IMO, that's the informed part of informed consent. Explaining outcome data is key, but giving the family/patient a choice is also key.
Psychoanalysis: Useful for self improvement but basically useless for any axis I diagnosis or borderline/antisocial stuff. It also seems to be the mental health's original pyramid scheme. Caveat: I am an analysand because personality traits both drive me to further education and treatment.
What's the intervention where you tell anxious or depressed patient to tap on their face?
This is called "Thought Field Therapy" which was invented by Richard Callahan. There was more than a bit of controversy about this crud. The "scientific support" for this "therapy" was a series of articles that were published in the Journal of Clinical Psychology without peer review. Cause that isn't strange. A few years later, the Delphi poll indicated that the therapy was probably discredited. It seems to be based on the idea that memories create a thing in the chi, and tapping disrupts the chi. The WHO has issued a statement that the concept of chi is not compatible with science. A session takes 15 minutes and training cost several grand.
- Joined
- Feb 15, 2009
- Messages
- 18,026
- Reaction score
- 23,767
Aricept: There was an article about 10 years ago about what patient's families want to know when getting diagnosed with dementias. IIRC, it was titled something like "the rule of three" with diagnosis, prognosis, and possible interventions being the three. IMO, that's the informed part of informed consent. Explaining outcome data is key, but giving the family/patient a choice is also key.
Psychoanalysis: Useful for self improvement but basically useless for any axis I diagnosis or borderline/antisocial stuff. It also seems to be the mental health's original pyramid scheme. Caveat: I am an analysand because personality traits both drive me to further education and treatment.
I still tell people about it, but I also tell them about the outcome literature. I know very few people who do. I encounter more families who come in saying, "Our Dr. said this would stop/slow down his dementia, but it doesn't seem to be working, he/she is getting worse!" No ****, the medication is useless, unless the patient is also constipated.
I'm still not even convinced in the self improvement part of psychoanalaysis. Haven't seen any meaningful outcome research on that aspect. Only a couple of study with outcome measures that are equally empirically untestable.
- Joined
- Apr 6, 2007
- Messages
- 10,827
- Reaction score
- 5,609
Caveat: I am an analysand because personality traits both drive me to further education and treatment.
This is all so Cats in the Cradle...
- Joined
- Oct 7, 2006
- Messages
- 22,382
- Reaction score
- 4,324
What's the intervention where you tell anxious or depressed patient to tap on their face? I had some of this nonsense yesterday...
I had a patient a few wks ago who's "therapist" was trained in EMDR….*roll eyes*….BUT…since the patient was still photophobic (from a slip and fall 1+ yrs ago…hold your groans), the eye movement stuff couldn't be done. Don't worry though, the "therapist" tapped on her thigh and the magic of EMDR….err…TTDR (Thigh Tap) was born! Trying something randomly and assuming it is working is research, right?
The above examples are why we push EBTs and proper training in graduate school.
- Joined
- Feb 15, 2009
- Messages
- 18,026
- Reaction score
- 23,767
That's the art part of the field, T4C. "I'm a painter, and the patient's mind is my palette."
- Joined
- Mar 24, 2014
- Messages
- 5,527
- Reaction score
- 6,556
You have consistently reported that aricept is not effective and you are more obviously more familiar with the research than myself, but I decided to look at some articles on it and am seeing articles that provide evidence that it does improve cognition. I am just wondering how to reconcile this. Here is an example from New England Journal of Medicine http://www.ncbi.nlm.nih.gov/pubmed/22397651I still tell people about it, but I also tell them about the outcome literature. I know very few people who do. I encounter more families who come in saying, "Our Dr. said this would stop/slow down his dementia, but it doesn't seem to be working, he/she is getting worse!" No ****, the medication is useless, unless the patient is also constipated.
I'm still not even convinced in the self improvement part of psychoanalaysis. Haven't seen any meaningful outcome research on that aspect. Only a couple of study with outcome measures that are equally empirically untestable.
D
deleted343839
Don't worry though, the "therapist" tapped on her thigh and the magic of EMDR….err…TTDR (Thigh Tap) was born!
Ingenious. If a patient asked me to tap their thighs we'd need to have a serious talk about boundaries. Now I know better.
D
deleted343839
You have consistently reported that aricept is not effective and you are more obviously more familiar with the research than myself, but I decided to look at some articles on it and am seeing articles that provide evidence that it does improve cognition. I am just wondering how to reconcile this. Here is an example from New England Journal of Medicine http://www.ncbi.nlm.nih.gov/pubmed/22397651
I think here we have an example of a drug that meets certain pre-defined endpoints on paper, but the endpoints are a low bar and don't necessarily translate to real-world benefit, especially in the face of a progressive disease.
- Joined
- Feb 15, 2009
- Messages
- 18,026
- Reaction score
- 23,767
You have consistently reported that aricept is not effective and you are more obviously more familiar with the research than myself, but I decided to look at some articles on it and am seeing articles that provide evidence that it does improve cognition. I am just wondering how to reconcile this. Here is an example from New England Journal of Medicine http://www.ncbi.nlm.nih.gov/pubmed/22397651
Few things. Probably the most important is that you need to know the difference between statistically significant change, and clinically significant change on the outcome measures used. Second, you also need to know how terrible the outcome measures used are. Generally it's a screening instrument with fairly wide test-retest values for interval change. When people have actually used more stringent measures, even the statistically significant stuff goes away. In general though, most of the larger studies show a statistical, yet clinically insignificant change up to 12 weeks, which then goes away. In the few studies that have looked at long term (up to 5 years) effects, there is no difference in time to institutionalization and no cost-saving benefit. Granted, there are only like 3 of these types of studies, so the data is limited on very long-term stuff.
Additionally, there is more data coming out on combining treatments. Those may show something, too soon to tell. But, the mono-therapy data is not encouraging when you look at it in total. It's especially non-encouraging when you only look at independent data outside of pharma funded research.
- Joined
- Oct 7, 2006
- Messages
- 22,382
- Reaction score
- 4,324
That's the art part of the field, T4C. "I'm a painter, and the patient's mind is my palette."
…and when that doesn't work REAL clinicians need to pick up the pieces.
In the past year I've seen:
1. A pt fresh from the Amen Clinic w. a giant print out of complete crap "testing". No improvements, but a new dx of ADHD amongst other things.
2. A pt who religiously does "neurofeedback" training on a weekly basis (for years)….no improvements.
3. A pt who currently sees a "christian therapist" to remove the demon in her (she has schizophrenia and then had a head injury).
4. Countless EMDR patients who haven't gotten better from their head injuries.
5. A pt seeing a naturpath (sp?) who prescribed all sorts of neutricuticals and junk science, her head injury hasn't improved.
6. A pt who saw a "therapist" for Reiki and some kind of laying of hands/energy healing treatment. She still has migraines.
7. A pt. who came from a well known quack chiropractic "concussion clinic". Similar printouts of junk science and a 5-figure bill. No change in head injury status or symptoms.
8. I've seen countless pts who sustained concussions and attended "eye therapy" with an optometrist to, "help balance out their brains." Hundreds/thousands of dollars later….no improvement.
The list can go on.
We might want to split these posts out to a new thread.
- Joined
- Oct 7, 2006
- Messages
- 22,382
- Reaction score
- 4,324
Additionally, there is more data coming out on combining treatments. Those may show something, too soon to tell. But, the mono-therapy data is not encouraging when you look at it in total. It's especially non-encouraging when you only look at independent data outside of pharma funded research.
I'm sitting on a mound of data that includes acute in-pt use of Aricept (and similar meds) in the treatment of moderate to severe brain injury; not dementia…but still clinically relevant. The stats are crazy complex to control for other factors (as this wasn't the primary aim of the study, but my carve out). I hope to get something out in the next ~2 years about it. I have 2-3 other manuscripts I'd like to get out first, as I think the data are more promising elsewhere.
- Joined
- Feb 15, 2009
- Messages
- 18,026
- Reaction score
- 23,767
Yeah, I'm not as familiar with outcome data on the use of it in actual brain injury. I'd be interested in what comes out of that data set. But yeah, I wouldn't want to have to control for all of those factors. Especially in mod-severe where the location of injury will play such a huge role in cognitive outcomes alone.
- Joined
- Oct 7, 2006
- Messages
- 22,382
- Reaction score
- 4,324
Yeah, I'm not as familiar with outcome data on the use of it in actual brain injury. I'd be interested in what comes out of that data set. But yeah, I wouldn't want to have to control for all of those factors. Especially in mod-severe where the location of injury will play such a huge role in cognitive outcomes alone.
I'm definitely leaning on the stats experts, who have taught me a lot about breaking down massive data. I just don't have the time right now, but I'm hoping at some point early next year I can round up a few folks on the study to start our next round of manuscripts.
- Joined
- Feb 10, 2008
- Messages
- 7,531
- Reaction score
- 6,693
What's the intervention where you tell anxious or depressed patient to tap on their face? I had some of this nonsense yesterday...
I do this when I have impacted sinuses, I guess it does make me feel I'm doing something for it.
Battle tapping? I've seen that one a lot in the VA.
- Joined
- Mar 24, 2014
- Messages
- 5,527
- Reaction score
- 6,556
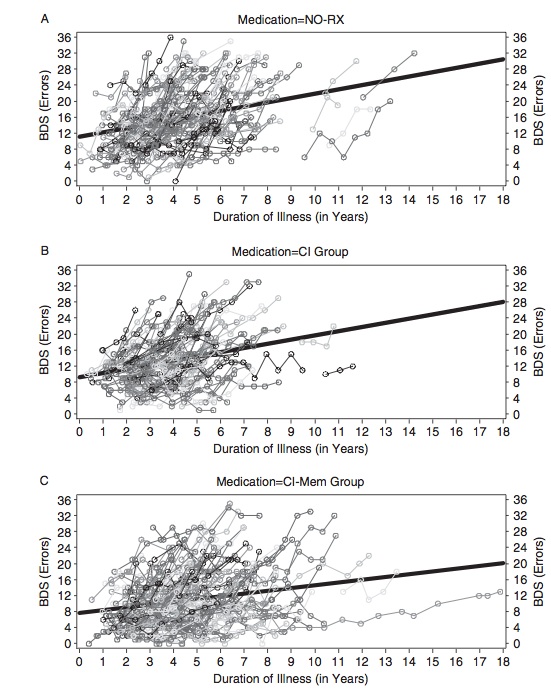
Thanks for the additional info. That jibes with my cursory review and as it isn't a current clinical concern, that will suffice. I used to stay up more on the neuro stuff but only have so much time and mental energy. Also, just wanted to add that I am very familiar with the distinction between clinical significance verses statistical significance and as I was perusing the web on this topic, I thought this image tells that story well. Also the BDS is the Blessed Dementia Scale (never heard of it myself) which am I safe in assuming would be the type of screening tool that is one of the poor outcome measures that you are referring to.Few things. Probably the most important is that you need to know the difference between statistically significant change, and clinically significant change on the outcome measures used. Second, you also need to know how terrible the outcome measures used are. Generally it's a screening instrument with fairly wide test-retest values for interval change. When people have actually used more stringent measures, even the statistically significant stuff goes away. In general though, most of the larger studies show a statistical, yet clinically insignificant change up to 12 weeks, which then goes away. In the few studies that have looked at long term (up to 5 years) effects, there is no difference in time to institutionalization and no cost-saving benefit. Granted, there are only like 3 of these types of studies, so the data is limited on very long-term stuff.
Additionally, there is more data coming out on combining treatments. Those may show something, too soon to tell. But, the mono-therapy data is not encouraging when you look at it in total. It's especially non-encouraging when you only look at independent data outside of pharma funded research.
In terms of prestige between the two..what do you guys think? Obv Physicians are more valued, but I'm not really sure where Psychologists stand as a whole. Sometimes you guys seem to suggest that everyone thinks they can do your job..but I would guess a lot of that is dependent on what specialty?
- Joined
- Oct 7, 2006
- Messages
- 22,382
- Reaction score
- 4,324
Prestige….it all depends on the setting you work and how you do what you do.
Financial security and access to jobs…leans very much to the physician side (for most specialities).
Financial security and access to jobs…leans very much to the physician side (for most specialities).
I don't think either psychology or medicine offers an inherent "prestige" anymore. Those days are long gone. I think it depends much more on setting and type of position. Psychologist or physician, you won't see much in the way of prestige in any sort of "generic" role (e.g. clinician churning through patients all day, run-of-the-mill academic, etc.).In terms of prestige between the two..what do you guys think? Obv Physicians are more valued, but I'm not really sure where Psychologists stand as a whole. Sometimes you guys seem to suggest that everyone thinks they can do your job..but I would guess a lot of that is dependent on what specialty?
- Joined
- Feb 15, 2009
- Messages
- 18,026
- Reaction score
- 23,767
Thanks for the additional info. That jibes with my cursory review and as it isn't a current clinical concern, that will suffice. I used to stay up more on the neuro stuff but only have so much time and mental energy. Also, just wanted to add that I am very familiar with the distinction between clinical significance verses statistical significance and as I was perusing the web on this topic, I thought this image tells that story well. Also the BDS is the Blessed Dementia Scale (never heard of it myself) which am I safe in assuming would be the type of screening tool that is one of the poor outcome measures that you are referring to.
Yeah, the study you posted shows that statistical difference, but that MMSE score is far away from being clinically significant by any metric. And yeah, the Blessed is roughly in the same category with the MMSE and the MoCA.
- Joined
- Jan 7, 2010
- Messages
- 9,319
- Reaction score
- 5,585
I've also seen it suggested in a paper or two that atorvastatin may improve cognitive functioning in folks with Alzheimer's dementia. No large scale and/or RCT-type studies that I know of, though. Have also seen it suggested that statins that are less lipophilic may be less cognitively-impacting.
As for prestige, like T4C mentioned, it'll depend in large part on where and how you work. And as Ollie said, the prestige of healthcare careers in general "ain't what it used to be." Which has some benefits, in that the power differential between provider and patient may feel lessened, and patients may then be less hesitant to ask questions and voice concerns regarding diagnoses and treatments.
As for prestige, like T4C mentioned, it'll depend in large part on where and how you work. And as Ollie said, the prestige of healthcare careers in general "ain't what it used to be." Which has some benefits, in that the power differential between provider and patient may feel lessened, and patients may then be less hesitant to ask questions and voice concerns regarding diagnoses and treatments.
- Joined
- Feb 15, 2009
- Messages
- 18,026
- Reaction score
- 23,767
Do most people you work with call you Dr? how about patients? do most patients even really understand the training of a neuropsychologist?
Yes, Yes, sometimes.
- Joined
- Oct 7, 2006
- Messages
- 22,382
- Reaction score
- 4,324
I've also seen it suggested in a paper or two that atorvastatin may improve cognitive functioning in folks with Alzheimer's dementia. No large scale and/or RCT-type studies that I know of, though. Have also seen it suggested that statins that are less lipophilic may be less cognitively-impacting.
I'll check those studies out, thanks!
As for prestige, like T4C mentioned, it'll depend in large part on where and how you work. And as Ollie said, the prestige of healthcare careers in general "ain't what it used to be." Which has some benefits, in that the power differential between provider and patient may feel lessened, and patients may then be less hesitant to ask questions and voice concerns regarding diagnoses and treatments.
As I mentioned, it depends on your job. I know private practice folks who have carved out a nice living, though aren't really "known" in the larger community. Maybe if they push to get on local tv and grow their brand, but that's the 0.01%. I know others who are more active academics and have some visibility, but it takes a lot of work. Most of the "well known" in the field of psychology are academics who have published prolifically.
Do most people you work with call you Dr? how about patients? do most patients even really understand the training of a neuropsychologist?
Yes. Yes. Rarely.
In a formal setting most staff/colleagues use titles, though it isn't a hard and fast rule.
Similar threads
- Replies
- 7
- Views
- 1K
